- Understanding Postpartum Depression and How to Overcome It
- 4 Ways to Cope with Postpartum Depression Anxiety During the Coronavirus Pandemic
- Here are four ways to help cope
- Worried someone you love may be suffering from PPD or PPA? Watch for these signs
- Next Steps Resources
- Postpartum depression
- What is postpartum depression
- How common is postpartum depression
- How do I know if I have postpartum depression?
- What causes postpartum depression
- Are some women more at risk of postpartum depression
- What is the difference between “baby blues” and postpartum depression
- What should I do if I have symptoms of postpartum depression
- What can I do at home to feel better while seeing a doctor for postpartum depression?
- How is postpartum depression treated
- What can happen if postpartum depression is not treated
- Did we answer your question about postpartum depression
- Sources
- Life hacks Dealing with postpartum depression
- Skin-to-skin contact
- Baby massage
- Smile
- Sing
- Postpartum Depression
- Overview
- What is postpartum depression
- What are the types of postpartum depression
- Who is affected by postpartum depression
- How do I know if I have baby blues or postpartum depression
- How long does postpartum depression last
- What factors increase my risk of being depressed after the birth of my child
- Symptoms and Causes
- What are the symptoms of postpartum depression
- What causes postpartum depression
- Can postpartum depression affect my baby
- Diagnosis and Tests
- How is postpartum depression diagnosed
- How do doctors screen for postpartum depression
- Management and Treatment
- How is postpartum depression treated
- What medications can I take for postpartum depression
- What are ways to cope with postpartum depression
- What happens if postpartum depression isn’t treated
- Prevention
- Can postpartum depression be prevented
- Outlook Prognosis
- What is the outlook for women with postpartum depression
- Living With
- When should I seek professional medical treatment for symptoms related to postpartum depression?
- Additional Common Questions
- Do I have postpartum anxiety or postpartum depression
- Can dads get postpartum depression?
- What is postpartum dysphoria
- How can I help someone with postpartum depression
- How to Manage and Cope with Postpartum Depression
Understanding Postpartum Depression and How to Overcome It
After the excitement and expectations of pregnancy, the reality of postpartum life can be a shock. The physical changes that start occurring even in the first few weeks after birth can be overwhelming. Added to that, the hormonal shifts and the mentally and emotionally taxing experience of caring for a newborn can leave many new mothers feeling unprepared and uncertain.
Postpartum depression is a common condition that affects many women after giving birth. It is important for new mothers to be aware of the signs and symptoms so they can seek help and support. It is normal to have some “baby blues” after birth, but when those symptoms last longer and start to impact daily life, it is likely that postpartum depression is present.
Postpartum depression is a form of depressive dysphoria that can be caused by a combination of factors, such as hormonal changes, sleep deprivation, and the stress of adjusting to a new role. Having a support system in place, including partners, family and friends, and healthcare providers, can help new mothers cope with these feelings.
If you or someone you know is experiencing postpartum depression, it is important to seek help. There are treatments and therapies available that can help manage and alleviate the symptoms of postpartum depression. Medications, such as selective serotonin reuptake inhibitors (SSRIs) and anti-anxiety medications, may be prescribed to help balance hormone levels and manage the depressive symptoms.
In addition to medication, there are also other forms of treatment that can be helpful. Talk therapy, support groups, and self-care practices, such as exercise and proper nutrition, can all contribute to the recovery and well-being of new mothers. It is important to remember to take care of yourself during this time and to not feel alone in your experience.
Postpartum depression is a common condition, but it is not something that women have to face alone. With the right support and access to resources, new mothers can get the help they need to manage their mental health and develop a strong bond with their baby. The key is to be realistic in your expectations and to seek help when you need it. Remember, postpartum depression is not a sign of weakness or failure, but rather a common condition that can be managed with the right support and care.
4 Ways to Cope with Postpartum Depression Anxiety During the Coronavirus Pandemic
Postpartum depression and anxiety can be challenging enough for new mothers, but the added stress and uncertainty of the coronavirus pandemic can make it even harder to manage. If you’re a new mom experiencing postpartum depression, here are four ways to cope with your symptoms during these difficult times:
|
1. Discuss your feelings |
Talking about your emotions and fears with a trusted friend or family member can provide valuable support and help you feel less alone. Even though physical distancing is important, maintaining social connections is crucial. |
|
2. Find online support groups |
Joining online support groups specifically for postpartum depression can connect you with other moms who are going through similar experiences. These groups can provide a space for sharing tips and advice, offering a sense of community. |
|
3. Stay engaged with your baby |
Despite feeling overwhelmed or worried, try to stay present and enjoy moments with your baby. Engaging in activities like cuddling, playing, or talking to your baby can help strengthen the bond between you and provide some relief from anxiety. |
|
4. Consider professional help |
If your symptoms are frequent, severe, or don’t improve with self-help strategies, it may be necessary to seek professional treatment. Your healthcare provider can recommend appropriate options, including therapy, medication, or contacting international postpartum centers for additional support. |
Remember, it’s important to prioritize your mental health and seek the support you need. Postpartum depression and anxiety are common and treatable. With the right care and assistance, you can manage your symptoms and experience the love and joy that comes with motherhood, even during these challenging times.
Here are four ways to help cope
Adjusting to life as a new mother can be a challenging and overwhelming experience. During this time, it is not uncommon for a woman to experience postpartum depression, a type of depression that can affect a woman’s mental and emotional well-being after giving birth. If you think you may be experiencing postpartum depression, it is important to seek help from a healthcare provider to develop a plan for managing your symptoms. Here are four ways that can assist you in coping with postpartum depression:
|
1. Prioritize self-care: As a new mother, it is essential to prioritize self-care. This can include things like getting enough sleep, eating nutritious meals, and engaging in activities that bring you joy. By taking care of yourself, you can improve your overall well-being and better manage the challenges that come with postpartum depression. |
2. Seek support from your community: Joining a postnatal support group or seeking support from other mothers can be incredibly beneficial. Being able to connect with others who are going through similar experiences can help you feel less alone and provide you with valuable resources and strategies for coping with postpartum depression. Consider reaching out to local community centers, online forums, or even your healthcare provider for recommendations. |
|
3. Communicate with your partner: It is important to have open and honest communication with your partner during this time. Your partner can provide emotional support and assist you with daily tasks. Involving your partner in your journey can help lighten the load and make you feel less overwhelmed. Together, you can develop strategies for managing postpartum depression and navigate this new chapter of your lives as parents. |
4. Consider therapy or counseling: If your postpartum depression is severe or if you feel like you need additional support, seeking therapy or counseling can be highly beneficial. A mental health professional, such as a certified therapist or psychologist, can help you explore the underlying causes of your depression and provide you with coping strategies tailored to your specific needs. Therapy sessions can be conducted individually or with your partner, depending on what you think would be most helpful for you. |
Remember, managing postpartum depression takes time and effort. It is important to be patient with yourself and know that it is okay to ask for help. By prioritizing self-care, seeking support, communicating with your partner, and considering therapy, you can develop effective strategies for coping with postpartum depression and improve your overall well-being.
Worried someone you love may be suffering from PPD or PPA? Watch for these signs
If you know someone who has recently given birth and you’re concerned that they may be experiencing postpartum depression (PPD) or postpartum anxiety (PPA), there are several signs to look out for. It’s essential to be informed so you can offer support and encourage them to seek professional help if needed.
- Feeling overwhelmed or hopeless: If your loved one seems to be struggling with feelings of sadness, hopelessness, or excessive guilt, it could be a sign of PPD or PPA.
- Difficulty bonding with the baby: Mothers with postpartum depression may find it challenging to connect emotionally with their newborn, which can lead to feelings of guilt or inadequacy.
- Extreme mood swings: If you notice drastic mood swings, such as going from happy to irritable or sad, it may be an indication of a postpartum mood disorder.
- Anxiety and panic attacks: PPA can manifest as excessive worry, feeling constantly on edge, or having frequent panic attacks.
- Changes in appetite and sleep patterns: Pay attention to any significant changes in eating and sleeping habits. PPD or PPA may cause a decrease or increase in appetite and disruptions in sleep.
- Decreased enjoyment in activities: Your loved one may lose interest in activities they once enjoyed and may have trouble feeling pleasure or happiness.
- Physical symptoms: PPD and PPA can also manifest as physical symptoms such as headaches, stomachaches, or low energy.
- Thoughts of hurting oneself or the baby: If your loved one expresses thoughts of self-harm or harming the baby, it’s crucial to take immediate action.
If you notice any of these signs, it’s important to encourage your loved one to speak with a healthcare provider. The best course of action may involve consulting with a therapist or psychiatrist who specializes in postpartum mood disorders. They can provide a proper diagnosis and recommend the most appropriate treatment options, which may include therapy, medication, or a combination of both.
Remember, postpartum depression and anxiety are treatable conditions. Your support and understanding can make a significant difference in helping your loved one on their path to recovery.
Next Steps Resources
When it comes to postpartum depression, it is important to seek help and attention. If you are experiencing symptoms such as anxiety, severe mood swings, or thoughts of death, it is crucial to reach out to a healthcare professional. Your physician can help determine the severity of your symptoms and recommend appropriate treatment options.
There are many resources available to support mothers who are dealing with postpartum depression. One option is therapy, which can be helpful in addressing the emotional difficulties that come with this condition. Additionally, anti-anxiety medications or selective serotonin reuptake inhibitors (SSRIs) can be prescribed to help improve mood and regulate brain chemical levels.
In addition to professional help, there are also various services that can assist with parenting and self-care. Many communities have support groups or counseling services specifically tailored to postpartum depression. These resources can provide a safe space to share experiences, ask questions, and receive advice from others who have gone through similar struggles.
It is crucial to keep in mind that postpartum depression is a real and valid condition. It is not something that should be dismissed or ignored. Caring for your mental health is just as important as caring for your physical health. Even though it might not always be easy, try to reach out to trusted friends or family members who can offer support and understanding.
Remember that you are not alone. Many people have experienced postpartum depression and have found ways to overcome it. If you ever feel overwhelmed or isolated, there are resources available to help. Don’t hesitate to reach out for support.
In terms of self-care, there are several things you can do to improve your mental health. Establish a routine that includes activities you enjoy, such as going for a walk or spending time doing a hobby. Eating a balanced diet and getting enough rest can also have a positive impact on your overall well-being.
When it comes to feeding your baby, it’s important to look for the best option that works for you and your baby. Whether you choose breastfeeding or using formula, make sure to seek advice from a healthcare professional. They can provide guidance and answer any questions you may have.
Lastly, don’t underestimate the power of a support network. Connect with other mothers who are going through similar experiences. Join online groups or follow relevant pages on social media platforms like Pinterest. Building a community of people who understand what you’re going through can make a world of difference.
Postpartum depression

Postpartum depression is a severe form of depression that occurs after giving birth. It is estimated that about 1 in 7 mothers experience postpartum depression. Since the symptoms can vary from person to person, it is important for new mothers to be aware of the signs and seek help if they suspect they are suffering from postpartum depression.
There are various strategies that can be used to cope with postpartum depression. Counseling with a licensed therapist can be very beneficial, as it provides a safe space to express and explore emotions. Psychotherapy, such as cognitive-behavioral therapy, can help mothers develop healthy coping mechanisms and improve their mental well-being.
In some cases, medication may also be necessary. Antidepressant medicine can help stabilize mood and alleviate symptoms of depression. However, it is important to consult with a physician before starting any medication, as it can have potential side effects and may not be safe for breastfeeding mothers.
Support from friends, family, and the community is crucial in helping mothers recover from postpartum depression. Creating a support system can provide a valuable network of people to lean on in times of need. Support groups, both in person and online, can also be beneficial, allowing mothers to connect with others who have experienced similar challenges.
Recognizing and responding to the signs of postpartum depression early on is essential. It is normal for new mothers to experience mood swings and feel tired, but if these symptoms persist for longer than a few weeks and interfere with daily life, it may be postpartum depression. Some common signs include feelings of sadness, hopelessness, and a lack of interest in activities once enjoyed.
Postpartum depression can also affect relationships. It may be harder for mothers to bond with their baby or maintain healthy relationships with their partner. Partners and other family members should be educated on the symptoms of postpartum depression so they can provide the necessary support.
Postpartum depression can be experienced by non-birthing parents as well. It is important to acknowledge that postpartum depression can affect anyone who is involved in the care of a new baby. Non-birthing parents should also be encouraged to seek help and support if needed.
In conclusion, postpartum depression is a serious condition that affects many new mothers. It is important for mothers to recognize the signs and seek help if needed. Strategies such as counseling, medication, and support from loved ones and the community can contribute to a healthy recovery.
What is postpartum depression
Postpartum depression is a type of mood disorder that many women face after giving birth. It is a warm and honest look at the reality of becoming a mother, which can often be overwhelming. The stress of taking care of a newborn, the hormonal changes that occur in the body, and the physical strain from childbirth can all contribute to the development of postpartum depression.
Postpartum depression goes beyond the “baby blues” that many women experience after giving birth. While the baby blues typically resolve on their own within a few weeks, postpartum depression is a more intense and prolonged condition that can last for several months or even longer. This type of depression is not easy to deal with and often requires professional help.
If you’re experiencing symptoms of postpartum depression, it’s important to reach out for support. Don’t feel guilty or hopeless. There are many treatments and strategies that can help you feel better. A therapist or counselor can recommend psychological interventions, such as therapy sessions or medication, to help stabilize your mood and decrease feelings of sadness, agitation, or hopelessness.
In some cases, a person may need to be hospitalized to receive immediate and intensive care. In severe cases of postpartum depression, a person may have thoughts of harming themselves or their baby. If you’re experiencing these thoughts, it’s important to seek help immediately. Contact your doctor, therapist, or a helpline to get the assistance you need.
It’s important to understand that postpartum depression is not your fault. It’s a medical condition that can be triggered by a combination of factors, including hormonal changes, lack of sleep, and stress. It’s also more likely to develop if you have a history of depression or other mental health disorders. However, it’s important to note that postpartum depression can affect anyone, regardless of their pre-pregnancy mental health.
If you suspect that you or someone you know has postpartum depression, it’s important to talk to a healthcare professional. Speak with your doctor, pediatrician, or a reproductive mental health specialist. They can diagnose postpartum depression based on your symptoms and may recommend tests to rule out other medical conditions.
In addition to seeking professional help, there are strategies that can be helpful for managing postpartum depression. These include engaging in self-care activities, such as getting enough sleep, eating a balanced diet rich in nutrients, and finding time for activities that you enjoy. It can also be helpful to focus on bonding with your baby through activities such as breastfeeding, using formula, or engaging in skin-to-skin contact to release oxytocin, a hormone that can help improve mood.
Support centers and support groups can also be a valuable resource for women experiencing postpartum depression. Connecting with other moms who have gone through or are going through similar experiences can provide a sense of community and understanding. Sharing experiences can help decrease feelings of isolation and guilt.
Remember, you’re not alone. Postpartum depression is a common condition that affects many women, but with the right support and treatment, it can be managed and overcome.
How common is postpartum depression
Postpartum depression is a common condition that affects many new mothers. It is estimated that up to four in ten women experience some form of postpartum depression. This condition can occur anytime within the first year after childbirth and is often accompanied by feelings of sadness, anxiety, irritability, and fatigue.
There are several factors that can contribute to the development of postpartum depression. Hormonal changes, such as a drop in estrogen and progesterone levels after giving birth, can have a significant impact on a woman’s mood and emotional well-being. Additionally, the sleep deprivation that often comes with caring for a newborn can leave new mothers feeling exhausted and overwhelmed.
Another factor that can contribute to postpartum depression is the adjustment to new responsibilities and changes in lifestyle that come with having a baby. Many women may find it difficult to adapt to the demands of breastfeeding, with concerns about milk supply, latching, and the overall experience. Some women may also feel worried or guilty about stopping breastfeeding, as it can be seen as the best option for the baby’s health.
It’s important to recognize the signs and symptoms of postpartum depression and seek help if you’re experiencing them. Some common signs of postpartum depression include persistent feelings of sadness, difficulty bonding with your baby, loss of interest in activities you once enjoyed, changes in appetite or sleep patterns, and frequent crying spells.
If you suspect you may have postpartum depression, it’s important to reach out to your healthcare provider. They can help identify your symptoms and develop a treatment plan that may include therapy, medication, or a combination of both. A certified therapist or counselor specializing in postpartum depression can provide you with the support you need to navigate this challenging time.
Support groups and online forums can also be a helpful resource for women affected by postpartum depression. Connecting with other mothers who are going through similar experiences can provide a sense of community and validation. International organizations, such as Postpartum Support International, offer online chat options and local support groups.
In addition to professional help and support from others, there are some strategies you can try to alleviate the symptoms of postpartum depression. Engaging in self-care activities, such as exercise, getting enough rest, and finding time for hobbies or activities you enjoy, can help improve your mood. It’s also important to be honest with yourself and others about your feelings and seek help when needed.
If you’re facing postpartum depression, remember that you’re not alone and there is help available. With the right support and treatment, you can overcome this condition and develop a strong bond with your baby.
How do I know if I have postpartum depression?
Postpartum depression is a serious condition that affects many new mothers. It is important to keep in mind that it is not a sign of weakness, and seeking support is essential. If you or anyone you know is experiencing symptoms that are related to postpartum depression, it is vital to reach out for help.
Knowing the signs and symptoms of postpartum depression is crucial. Some common indicators include feeling sad or down most of the time, losing interest in activities you used to enjoy, excessive crying, feeling hopeless or worthless, having difficulty bonding with your baby, experiencing extreme highs and lows, feeling anxious or panicky, having difficulty sleeping, struggling with appetite changes, feeling guilty or ashamed, having thoughts of hurting yourself or your baby, or feeling overwhelmed and unable to cope.
If you are seeing these symptoms in yourself or a loved one, it is important to seek professional help. A healthcare provider can diagnose postpartum depression and recommend the best course of treatment, which may include therapy, support groups, or medication.
In some cases, medication may be prescribed to help manage the symptoms of postpartum depression. Antidepressant medications work by balancing chemicals in the brain, which can help to improve mood and decrease feelings of anxiety and agitation. It is important to note that the decision to take medication should be made in consultation with a healthcare provider, weighing the potential risks and benefits for both the mother and the baby.
There are also several steps you can take to support your own mental health and well-being during this challenging time. Learning about postpartum depression, reaching out for support, and practicing self-care are all important strategies. Connecting with others who have experienced postpartum depression can be helpful, as they can provide an understanding ear and share coping strategies.
In addition to seeking professional help and support, there are several things you can do at home to help manage postpartum depression. Taking care of your own physical health is important, as exercise and a balanced diet can have a positive impact on your mental state. Engaging in activities that bring you joy and practicing relaxation techniques, such as deep breathing and meditation, can also help reduce symptoms of anxiety and stress.
Some additional recommendations include maintaining a consistent sleep schedule, getting as much rest as possible, and asking for help with tasks that feel overwhelming. It can also be beneficial to prioritize self-care by setting aside time to do things that make you feel good, whether that’s taking a bath, reading a book, or going for a walk.
If your symptoms are severe or not improving, make sure to reach out to a healthcare provider for further evaluation and support. Remember, you are not alone in this, and with the right treatment and support, postpartum depression can be managed effectively.
It is important to note that postpartum depression can also affect partners, not just mothers. Partners may experience symptoms such as feeling overwhelmed, having difficulty bonding with the baby, feeling irritable or angry, or having changes in appetite and sleep patterns. Partners should reach out for support as well, and considering seeking professional help can be beneficial for their own mental health.
If you or a loved one is experiencing symptoms of postpartum depression, it is crucial to talk about them and seek help. It is not a sign of weakness or failure as a parent. Reach out to healthcare providers, support groups, or other trusted individuals for assistance. Remember, there is help available, and you are not alone.
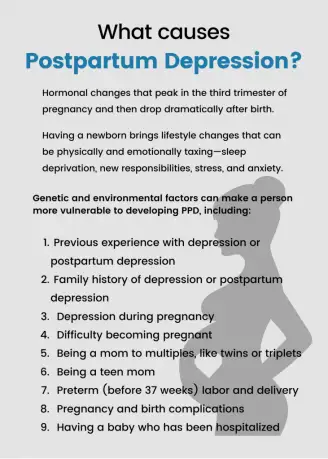
What causes postpartum depression
Postpartum depression (PPD) is a common mental health disorder that affects many new mothers worldwide. There are several factors that can contribute to the development of PPD:
- Hormonal changes: After childbirth, hormone levels in a woman’s body significantly fluctuate. These hormonal changes can affect brain chemistry and contribute to the development of PPD.
- Physical and emotional stress: The arrival of a new baby can be incredibly stressful, both physically and emotionally. The lack of sleep, the demands of caring for a newborn, and the loss of personal freedom and independence can all contribute to the development of PPD.
- Previous mental health issues: Women who have a history of depression, anxiety, or other mental health disorders are more likely to develop PPD.
- Lack of social support: Feeling isolated and lacking support from family, friends, or partners can increase the risk of developing PPD.
- Poor self-esteem: Some women may struggle with feelings of inadequacy or low self-worth after childbirth, which can contribute to the development of PPD.
- Pregnancy or childbirth complications: Women who experience complications during pregnancy or childbirth, such as a difficult labor, health problems for the baby, or postpartum complications, may have an increased risk of developing PPD.
- Psychological factors: Some women may have a particular personality type or underlying psychological issues that make them more susceptible to developing PPD.
- Lack of sleep and self-care: The constant sleep deprivation and neglecting self-care can further exacerbate symptoms of depression and increase the risk of developing PPD.
If you suspect that you or a loved one may be experiencing postpartum depression, it is important to seek help from a healthcare professional. Treatment options, such as therapy and medication, can be effective in managing PPD and helping women navigate this challenging period in their lives.
Are some women more at risk of postpartum depression
Postpartum depression is a serious mental health condition that affects many new mothers. While anyone can develop postpartum depression, some women may face a higher risk than others. Several factors can contribute to this increased risk.
- Previous experience with depression: Women who have experienced depression in the past are at a higher risk of developing postpartum depression. The hormonal changes during pregnancy and after childbirth can trigger depressive episodes.
- History of anxiety disorders: Women who have a history of anxiety disorders may be more susceptible to postpartum depression. The stress and hormonal changes during pregnancy and the postpartum period can exacerbate anxiety symptoms.
- Unplanned pregnancy: Women who feel overwhelmed or unprepared for pregnancy and motherhood may be more likely to experience postpartum depression. The lack of control and feelings of being trapped can contribute to the development of depressive symptoms.
- Limited social support: Lack of support from friends, family, or a partner can increase the risk of postpartum depression. Women who feel isolated and have limited access to a support system may find it more difficult to manage the challenges of motherhood.
- Hormonal changes: Hormones, such as oxytocin, play a significant role in mood regulation. Fluctuations in hormone levels during pregnancy and postpartum can contribute to mood swings and depressive symptoms.
- Difficulty adjusting to motherhood: The transition to motherhood is a significant life change that can be overwhelming and challenging. Some women may find it difficult to adjust to their new role and responsibilities, increasing their vulnerability to postpartum depression.
If you’re pregnant or have recently given birth and you’re concerned about the risk of postpartum depression, it’s essential to speak with your healthcare provider. Your physician or OBGYN can provide guidance, support, and appropriate treatment options.
Joining a support group or community of new mothers can also be beneficial. Talking with others who are going through similar experiences can help alleviate feelings of isolation and provide a space for honest discussions about postpartum depression.
Managing stress and practicing self-care strategies are crucial in reducing the risk of postpartum depression. Some strategies that may be helpful include meditating, regular exercise, getting enough sleep, and seeking therapy or counseling.
Remember, postpartum depression is a common condition that affects many new mothers. If you’re experiencing symptoms or feel overwhelmed, reach out for help. You’re not alone, and there are resources available to support you during this challenging time.
What is the difference between “baby blues” and postpartum depression

Having a baby is a major life event that brings a mix of emotions, both positive and negative. It’s not uncommon for new mothers to experience mood changes, including feeling a bit down or weepy. These feelings are often referred to as the “baby blues” and are a normal response to the hormonal changes and challenges of new parenthood. Baby blues usually occur within the first few days after giving birth and typically resolve on their own within a week or two.
Postpartum depression, on the other hand, is a more severe and persistent form of depression that occurs after childbirth. Unlike baby blues, postpartum depression is not a normal part of the postnatal period and requires treatment. It is estimated that around 10-20% of women experience postpartum depression, with symptoms typically appearing within the first month after giving birth. However, postpartum depression can develop any time within the first year.
The signs and symptoms of postpartum depression can include:
- Feeling sad, empty, or hopeless
- Loss of interest in activities or hobbies
- Frequent crying
- Changes in appetite or sleep patterns
- Difficulty bonding with the baby
- Feeling overwhelmed or panicked
- Extreme irritability or anger
- Feeling guilty or worthless
- Lack of energy or motivation
- Trouble concentrating or making decisions
While baby blues are generally considered to be a normal adjustment period, postpartum depression is a more serious mental health condition that can have a significant impact on a woman’s well-being and ability to function. It is important to seek help if you think you may be experiencing postpartum depression, regardless of the time frame since giving birth.
The exact cause of postpartum depression is unknown, but it is believed to be a combination of physical, emotional, and environmental factors. Hormonal changes, such as a sudden drop in reproductive hormones after childbirth, can play a role. Other factors that can contribute to postpartum depression include a history of depression or anxiety, a lack of support from family or friends, and high levels of stress.
Treatment for postpartum depression can include therapy, medication, or a combination of both. Self-care strategies, such as getting enough sleep, eating well, and finding time for yourself, are also important. It’s crucial to reach out to a healthcare professional for help and support. Remember, seeking treatment for postpartum depression does not mean you are a bad parent or that you don’t love your baby. It means you are taking the necessary steps to prioritize your mental health and well-being.
What should I do if I have symptoms of postpartum depression
If you are mentally struggling after giving birth and experiencing symptoms of postpartum depression, it’s important to reach out for support. Here are some steps you can take:
- Recognize the symptoms: It’s crucial to know the signs of postpartum depression, such as feelings of sadness, irritability, and loss of interest in activities you once enjoyed.
- Talk to your healthcare provider: Schedule an appointment with your healthcare provider to discuss your symptoms in detail. They can provide guidance and work with you to develop a treatment plan.
- Don’t panic: Remember that postpartum depression is a common condition and you are not alone. Many other new mothers experience similar feelings.
- Seek social support: Reach out to friends, family, or support groups who can provide emotional support during this challenging time.
- Take care of yourself: Make sure you are eating nutritious meals, getting enough rest, and engaging in activities that you enjoy.
- Create a bond with your baby: Practice skin-to-skin contact and engage in activities that promote bonding, such as breastfeeding and playing with your baby.
- Consider professional help: If your symptoms worsen or do not improve after a few weeks, it may be beneficial to seek help from a mental health professional who specializes in postpartum depression.
- Discuss treatment options: Talk to your healthcare provider about various treatment options, such as therapy, support groups, or medication.
- Stay informed: Read books, watch videos, or access reliable online resources to educate yourself about postpartum depression and the available support services.
- Keep an eye on your overall health: Postpartum depression can affect your physical health as well. Discuss any concerns with your healthcare provider.
- Stay connected: Maintain healthy relationships with your partner, friends, and family members, as these connections can provide much-needed support.
- Engage in hobbies or activities: Find time for activities that you enjoy and that bring you joy. This can help alleviate feelings of loneliness or emptiness.
- Understand the role of hormones: Hormonal changes that occur after childbirth can contribute to postpartum depression. Know that these changes are normal and treatable.
- Reach out to support centers: There are many support centers and organizations that specialize in postpartum depression. They can provide valuable resources and guidance.
- Don’t stop taking care of yourself: Remember that your well-being is just as important as taking care of your baby. Taking time for self-care is essential.
- Don’t hesitate to ask for help: If you feel overwhelmed or unable to cope, do not hesitate to seek help. There are trained professionals and helplines available to support you.
- Know that it’s okay to cry: Crying is a normal release of emotions and can be a healthy way to cope with postpartum depression. Give yourself permission to cry when you need to.
- Focus on the needs of your baby: Remember that taking care of your baby’s needs can also contribute to your own well-being. Engage in activities that nurture the bond between you and your baby.
- Identify contributing factors: Recognize any other factors that may be contributing to your postpartum depression, such as sleep deprivation or lack of support.
- Reach out to non-birthing partners: Postpartum depression can also affect non-birthing partners. If you are a non-birthing partner, it’s important to seek support for yourself as well.
- Don’t isolate yourself: Avoid isolating yourself from others. Maintain social connections and reach out to loved ones for support.
- Discuss medication options: In some cases, medication may be necessary to manage postpartum depression symptoms. Talk to your healthcare provider about medication options.
- Consider reproductive health: Postpartum depression can occur after any type of childbirth, including miscarriage or stillbirth. If you have experienced such events, it’s important to discuss the impact on your mental health with your healthcare provider.
- Stay hopeful: Remember that postpartum depression is treatable, and with the right support and treatment, you can overcome it.
- Reach out for a lifeline: If you or anyone you know is in immediate danger, such as having thoughts of self-harm or harm to others, call emergency services or a helpline right away.
Remember, it’s essential to reach out for support and take care of your mental health. You deserve to feel better and enjoy the precious moments with your baby.
What can I do at home to feel better while seeing a doctor for postpartum depression?
Postpartum depression is a serious condition that can affect new mothers after childbirth. If you are experiencing symptoms of postpartum depression, it is important to seek professional help, but there are also things you can do at home to help improve your well-being. Here are some options to consider:
- Recognize the signs: Learn about the symptoms of postpartum depression so that you can identify them in yourself. This knowledge will also help you understand what you are going through.
- Get support: Reach out to friends and family who can provide emotional support. Having a support system can make a big difference in your recovery.
- Establish a routine: Setting a daily routine can help give structure to your day, increasing your sense of control and stability.
- Take care of yourself: Make sure to prioritize self-care. This includes eating well-balanced meals, getting regular exercise, and getting enough sleep.
- Talk to a therapist: Consider seeing a therapist who specializes in postpartum depression. They can provide professional guidance and help you work through your feelings.
- Practice relaxation techniques: Try meditation, deep breathing exercises, or yoga to help alleviate stress and promote relaxation.
- Watch for warning signs: Pay attention to any thoughts of harming yourself or your baby, as well as any feelings of hopelessness or guilt. If you experience these thoughts, seek immediate medical attention.
- Learn about bonding: Educate yourself about bonding with your baby. While postpartum depression can affect the bonding process, there are ways to promote a strong relationship with your child.
- Read helpful material: Look for books or articles about postpartum depression to gain a better understanding of the condition and find useful tips for coping.
- Join a support group: Consider joining a support group for mothers with postpartum depression. Sharing experiences with others who are going through something similar can be comforting.
- Discuss treatment options: Talk to your doctor about the different treatment options available for postpartum depression. Medications or therapy may be recommended to help improve your symptoms.
- Take screenings seriously: If your doctor recommends a postpartum depression screening, take it seriously. Screening can provide valuable insights into your condition and help guide your treatment.
- Stay informed: Keep yourself updated on the latest research and developments in postpartum depression treatment. New therapies or techniques may become available that could improve your outlook.
- Avoid isolation: While it may be difficult to socialize when you are feeling down, try to connect with others. Loneliness can exacerbate feelings of depression.
- Watch your blood sugar: Keeping your blood sugar levels stable may help improve your mood. Eat regular, well-balanced meals and avoid excessive sugar intake.
- Take a break: It’s important to give yourself a break when you need it. Ask for help and take time for yourself, even if it’s just for a short walk or a relaxing bath.
- Limit exposure to negative material: Try to minimize exposure to media or material that may negatively affect your mood. Instead, focus on uplifting and positive content.
- Consider alternative therapies: Some people find relief from postpartum depression symptoms through alternative therapies such as acupuncture or massage. Talk to your doctor about these options.
- Find joy in small things: Look for small moments of joy and try to appreciate them. Whether it’s a smile from your baby or a beautiful sunrise, finding happiness in the little things can help improve your mood.
Remember, postpartum depression can be a challenging and difficult experience, but with the right support and treatment, you can recover and enjoy a fulfilling life with your new child.
How is postpartum depression treated
Postpartum depression can be a challenging experience for new mothers, but it is important to remember that there is help available. Here are some approaches that can be used to treat postpartum depression:
- Bonding: Creating a strong parent-child bond can help alleviate symptoms of postpartum depression. Spending quality time with your baby and engaging in activities together can contribute to this bond.
- Talk therapy: Speaking with a therapist can provide a safe space to discuss and process your feelings. Therapy can help identify any underlying issues and develop coping strategies.
- Medication: In more severe cases, medication may be prescribed to help regulate mood. Antidepressants can be prescribed to help manage symptoms of postpartum depression.
- Support groups: Connecting with others who have experienced postpartum depression can be helpful. Sharing experiences and advice with others who can relate to your situation can provide a sense of understanding and support.
- Lifestyle changes: Making changes to your daily routine and self-care can also have a positive impact on postpartum depression. This may include getting regular exercise, eating a healthy diet, and ensuring adequate sleep.
- Hormone therapy: Hormonal changes can contribute to postpartum depression. Hormone therapy, such as the use of brexanolone, may be prescribed to help regulate these hormones and alleviate symptoms.
- Professional help: If the symptoms of postpartum depression are severe or if thoughts of self-harm or harm to the baby are present, immediate professional help should be sought. A healthcare professional or therapist can provide the necessary support and guidance.
- International helplines and online resources: Access to support is available worldwide with various helplines and online resources. Numerous organizations and hotlines offer assistance and guidance for individuals experiencing postpartum depression.
- Postnatal classes and workshops: Participating in postnatal classes and workshops can provide education on postpartum depression and offer guidance on managing the challenges of motherhood.
Remember, it is essential to reach out for help if you are experiencing postpartum depression. With the right support and treatment, postpartum depression can be managed, and a person can regain their ability to enjoy motherhood and life overall.
What can happen if postpartum depression is not treated
Postpartum depression is a serious mental health condition that affects many new mothers. If left untreated, it can have profound effects on both the mother and her family.
Socially, untreated postpartum depression can lead to isolation and withdrawal from friends and loved ones. A mother suffering from depression may find it difficult to interact with others, leading to a strain on relationships and a sense of being alone in the world.
Medications are available that can help alleviate the symptoms of postpartum depression, but if a mother doesn’t seek treatment, she may continue to suffer needlessly. Symptoms like frequent crying, agitation, and hopelessness can make it challenging to cope with the demands of parenting and everyday life.
Postpartum depression can also affect the bond between a mother and her baby. If not treated, the lack of emotional connection may lead to difficulties in development and learning for the child. The baby may not receive the love and care they need, which can have long-term consequences on their well-being.
Physically, the effects of postpartum depression can be just as significant. Sleep deprivation is common for new mothers, but it becomes much more challenging when coupled with the symptoms of depression. Lack of sleep and constant fatigue can make it harder to function and care for a new baby.
Untreated postpartum depression can also increase the risk of other mental health disorders. Anxiety, panic disorder, and even thoughts of self-harm or suicide may develop if the depression is not addressed and treated.
It is essential for new mothers to reach out for help if they suspect they may be experiencing postpartum depression. Licensed therapists and counselors can provide psychotherapy to help mothers cope with their feelings and develop effective ways of managing stress and expectations.
In some cases, medication may be prescribed to help manage the symptoms of depression. Antidepressants can be safe and effective for breastfeeding mothers, but it is essential to speak with a pediatrician or mental health professional to determine the best treatment option.
Additionally, support from friends, loved ones, and support groups can be immensely helpful in overcoming postpartum depression. Knowing that others have experienced similar feelings and difficulties can provide hope and encouragement.
In conclusion, if left untreated, postpartum depression can have serious and lasting effects on a mother’s well-being, her family, and her child’s development. It’s crucial to seek help and support to ensure a healthy and happy postpartum experience.
Did we answer your question about postpartum depression
Postpartum depression is a common condition that affects many new mothers, and it is important to seek help if you think you may be experiencing symptoms. It’s easy to feel overwhelmed and worried about your mental health, especially if you’re a first-time mom. You might start feeling extreme sadness, loss of interest in things you used to enjoy, extreme fatigue, difficulty bonding with your baby, and even thoughts of harming yourself or your baby. If you are experiencing any of these symptoms, it is important to reach out to a medical professional who can offer the support and guidance you need.
There are many treatment options available for postpartum depression, including therapy, medication, and support groups. Therapy can be extremely helpful in helping you manage your symptoms and develop coping mechanisms. Medication can also be a very effective option for some women, especially those with more severe cases of postpartum depression or who are struggling to function in their daily life. It’s important to remember that there is no shame in seeking help and that getting the right treatment is crucial for both you and your baby’s well-being.
Research suggests that the hormone levels in a woman’s body after birthing can contribute to postpartum depression, so it’s not something that you can simply “snap out of.” It is a legitimate medical condition that needs to be taken seriously. It’s also important to note that postpartum depression can occur any time within the first year after giving birth, so it’s important to be aware of the signs and symptoms throughout that time frame.
Many new mothers also face a condition called postpartum anxiety, which is similar to postpartum depression but is more focused on intense worry and fear rather than extreme sadness. It is important to remember that there is no “right” way to feel after having a baby, and every mother’s experience is different. Some women may quickly develop a bond with their baby, while others may take more time. It’s important to give yourself permission to feel however you feel and to not compare yourself to other mothers.
Support from family and friends can also be crucial during this time. It’s important to have people in your life who can offer emotional support and help you with the day-to-day tasks of caring for a newborn. It’s also important to remember that self-care is not selfish and that taking care of your own physical and mental health is necessary in order to be the best mother you can be.
If you are worried about postpartum depression or have any questions, it’s important to reach out to a certified healthcare professional who can provide the guidance and support you need. Remember that you are not alone and that there are many resources available to help you through this challenging time.
Sources
Postpartum depression (PPD) is a serious condition that affects many new mothers. It is important to seek out sources of information and support in order to learn how to recognize and cope with this type of depressive disorder. Here are some helpful resources:
| The American College of Obstetricians and Gynecologists (ACOG) | The ACOG provides resources for perinatal mental health, including information on postpartum depression and how to best support someone who may be experiencing it. |
| National Institute of Mental Health (NIMH) | The NIMH offers resources on postpartum depression, including videos and fact sheets that can be useful in understanding the condition and finding appropriate treatment options. |
| Postpartum Support International (PSI) | PSI is a non-profit organization that provides support and resources for women and families experiencing perinatal mood and anxiety disorders. They have a helpline that can be reached at 1-800-944-4773. |
| Friends and Loved Ones | Having a support system is crucial for women with postpartum depression. Friends and loved ones can offer emotional support, help with childcare, and encourage seeking professional help. |
| Healthcare Providers | Obstetricians, gynecologists, and other healthcare providers can offer advice, diagnose PPD, and provide necessary treatment options. They can also refer patients to specialists if needed. |
It is important to remember that seeking help and support is not a sign of weakness. Postpartum depression is a medical condition that can be treated. With the right resources and support system in place, women can learn to cope with the challenges and enjoy a healthy and happy parenting journey.
Life hacks Dealing with postpartum depression
Postpartum depression (PPD) is a common condition that affects many new mothers. It can manifest in a variety of ways and have a significant impact on a woman’s emotional well-being. Here are some life hacks that can help with dealing with postpartum depression:
- Seek professional help: If you’re experiencing symptoms of postpartum depression, it’s essential to reach out to a healthcare provider. A physician or a mental health professional can provide the necessary support and treatment options.
- Join support groups: Connecting with others who are going through similar experiences can be incredibly helpful. Online forums and local support groups offer a space for sharing stories, asking questions, and receiving support from others who understand what you’re going through.
- Take care of your physical health: Physical exercise, a healthy diet, and adequate sleep can greatly contribute to your overall well-being. Regular exercise releases endorphins and helps reduce stress levels, while proper nutrition provides the essential nutrients your body needs.
- Ask for help: Don’t be afraid to ask for assistance with household chores or running errands. Partners, family members, or friends can lend a hand, allowing you to focus on self-care and bonding with your baby.
- Explore free resources: Many healthcare providers and organizations offer free resources for new mothers dealing with postpartum depression. These can include online chat services, helplines, and educational materials.
- Consider therapy options: Therapy sessions can be beneficial in helping you navigate the challenges of postpartum depression. Cognitive-behavioral therapy (CBT) and other forms of therapy can provide coping mechanisms and tools to manage the symptoms.
- Learn about the risks and warning signs: Educate yourself about the signs and symptoms of postpartum depression, as well as the potential risks associated with it. Being informed can help you recognize when you might need additional support or treatment.
- Practice self-care: Remember to take some time for yourself. Engage in activities that you enjoy, such as reading a book, meditating, or taking a relaxing bath. Self-care helps replenish your energy and reduces stress levels.
- Reach out to loved ones: It’s crucial to maintain social connections during this time. Reach out to your friends, family, or support network and let them know how you’re feeling. Simply talking to someone who cares can make a significant difference.
- Utilize available services: Take advantage of services provided by community organizations or healthcare providers. Some centers offer free or low-cost parenting classes, which can give you additional knowledge and support.
Remember, postpartum depression is a treatable condition, and with the right tools and support, you can overcome it. Don’t hesitate to seek help and reach out to others for support.
Skin-to-skin contact
Skin-to-skin contact, also known as kangaroo care, is a practice that involves placing a newborn baby naked, except for a diaper, on the bare chest of their parent or caregiver. This immediate and intimate contact has been shown to have many benefits for both the baby and the parent.
Research suggests that skin-to-skin contact can help newborns regulate their body temperature, heart rate, and breathing. It can also promote the release of hormones that aid in breastfeeding and bonding. Mothers who engage in skin-to-skin contact are more likely to breastfeed successfully and for a longer duration.
For fathers and non-birthing parents, skin-to-skin contact provides an opportunity to develop a close relationship with their newborn. It allows them to participate in caregiving activities and establish a strong bond with their child. Skin-to-skin contact can also foster feelings of self-confidence and competence in parenting.
In addition to its immediate benefits, skin-to-skin contact has been found to have long-term positive effects on the child’s development. Research has shown that babies who experienced frequent skin-to-skin contact in the early postnatal period have better cognitive and socioemotional outcomes later in life.
Skin-to-skin contact can also be beneficial for the parent’s mental health, particularly for those at risk of postpartum depression. The physical closeness and release of hormones during skin-to-skin contact can help regulate mood swings and reduce anxiety. It promotes feelings of relaxation and well-being, and may contribute to a faster recovery from childbirth.
Furthermore, skin-to-skin contact provides an opportunity for the parent to observe and respond to the baby’s cues and needs more quickly. This helps in building a strong caregiving relationship and enhances the parent’s confidence in their ability to understand and meet their baby’s needs.
Healthcare providers can encourage and support skin-to-skin contact as a preventive measure for postpartum depression. Including it as part of routine care can help parents feel more confident in their abilities and allow for early detection of signs of depression.
In cases where the mother is experiencing severe postpartum depression or psychosis, skin-to-skin contact may not be possible or recommended. In such situations, healthcare providers will need to explore other treatment options and provide support to the mother.
In conclusion, skin-to-skin contact is a simple yet powerful practice that can improve the health and well-being of both the baby and the parent. It is a valuable tool for promoting bonding, breastfeeding, and emotional well-being. All parents should be encouraged to engage in skin-to-skin contact with their newborns to reap its numerous benefits.
Baby massage
Massage is not just a great way to relax and unwind; it can also have many benefits for your baby’s well-being. Baby massage has been practiced for centuries and is believed to provide a range of physical and emotional benefits for both the baby and the mother. It is recommended for babies who are at least a few months old and can be continued throughout their early years.
Baby massage is a way for parents to bond and connect with their baby, providing a soothing and comforting touch. It can help reduce symptoms of postpartum depression in new mothers by promoting relaxation and reducing stress. The act of massaging the baby stimulates the release of hormones such as oxytocin, which enhances feelings of love and attachment in both the mother and the baby.
In addition to the emotional benefits, baby massage also provides physical benefits. It helps to stimulate the baby’s muscles, improve circulation, and promote better sleep. Massage can also aid digestion and ease discomfort caused by gases or constipation. By massaging the baby’s skin, it helps to strengthen their immune system and provides the necessary nutrients that their body needs.
Some studies have shown that babies who receive regular massage have improved cognitive development and higher IQ scores later in life. This is believed to be due to the positive effect of touch and stimulation on the baby’s brain development. Baby massage is also beneficial for babies with special needs, such as those with hearing impairments or developmental disabilities.
While it is easy to learn basic massage techniques, it is always a good idea to seek guidance from a professional or join a baby massage class. These classes provide not only the knowledge and skills but also a supportive environment where parents can share their experiences and concerns with other parents. It is important to note that baby massage should not be performed if the baby has any skin conditions or infections.
Although baby massage is a great way to bond with your little one, it is important to be aware of the potential risks. Certain factors, such as a history of perinatal depressive disorders or a lack of social support, can increase the risk of developing postpartum depression. It is also essential to maintain a proper balance and not rely solely on baby massage as a treatment for postpartum depression. If you’re feeling symptoms of depression, it is important to reach out to a healthcare provider who can offer counseling or prescribe medication like brexanolone, if needed.
In conclusion, baby massage is a wonderful way to promote bonding and support your baby’s overall well-being. It offers numerous physical and emotional benefits, both for the baby and the parent. Remember to take care of yourself as well, and if you or someone you know is struggling with postpartum depression, seek professional help. You don’t have to go through it alone, and there are effective treatments available.
Smile
Recognize the importance of a smile in the context of postpartum depression. Although it may seem like a small gesture, a smile can have a great impact on the mental health of new mothers. Postpartum depression is a severe condition that affects many women after giving birth, causing feelings of sadness, lack of energy, and stress.
Joining a support group or seeking professional help can be a great step towards overcoming postpartum depression. It is important for new mothers to know that they are not alone and that there are resources available to help them through this challenging time.
Newborn babies respond positively to their mother’s smile, as it is a warm and loving gesture. A smile can help create a strong attachment between the mother and baby and promote healthy emotional development. Furthermore, smiling releases hormones that make both the mother and baby feel happy, reducing stress levels and promoting a sense of well-being.
It’s important to look after oneself during this difficult period. Eating healthy meals and practicing self-care can help manage symptoms of postpartum depression. Lack of sleep can worsen feelings of depression and anxiety, so it’s vital to prioritize rest and find ways to improve sleep quality.
For some women, postpartum depression can be a serious condition that requires antidepressants to manage. However, it’s crucial to consult a healthcare professional before starting or stopping any medication, especially if they’re breastfeeding.
Screening for postpartum depression is an essential part of maternal healthcare. Many healthcare departments offer free screening for postpartum depression as part of routine check-ups. This allows healthcare providers to identify and support women who may be experiencing postpartum depression, ensuring their safety and well-being.
| Tips for Managing Postpartum Depression: |
|---|
| – Seek professional advice: It’s important to reach out to a healthcare professional or therapist who specializes in perinatal mental healthcare. |
| – Talk to someone: Sharing feelings with trusted family members or friends can be helpful for emotional support. |
| – Set realistic expectations: Adjusting to life with a newborn can be challenging, so it’s essential to be patient with oneself and set achievable goals. |
| – Practice self-care: Taking time for oneself, engaging in activities that bring joy, and prioritizing self-care can help alleviate symptoms of postpartum depression. |
| – Get enough rest: Lack of sleep can exacerbate symptoms of depression, so finding ways to improve sleep quality and getting enough rest is crucial. |
| – Form an attachment with the baby: Spending quality time bonding with the baby through activities such as skin-to-skin contact, breastfeeding, and playing can enhance the parent-child relationship and promote emotional well-being. |
| – Reach out for support: Joining support groups, both in-person and online, can connect new mothers with others who are going through similar experiences and provide a sense of community. |
| – Focus on the positive: Try to find joy in the small moments, celebrate accomplishments, and remind oneself that being a mother is a valuable and fulfilling role. |
| – Be patient: Recovery from postpartum depression takes time, and everyone’s journey is different. It’s important to be patient and kind to oneself throughout the process. |
In conclusion, postpartum depression can be a challenging and overwhelming experience for new mothers. However, with proper support, access to healthcare, and proactive self-care, it is possible to overcome and recover from this condition. Remember, you are not alone, and there are resources available to help you through this incredible journey of motherhood.
Sing
When it comes to dealing with postpartum depression, there are many strategies that can help alleviate symptoms and improve mood. One surprising and effective strategy is simply singing. Singing can help in many ways, including emotionally and physically.
Emotionally, singing releases oxytocin, a hormone that promotes feelings of happiness and bonding. When someone feels hopeless or depressed, singing can help increase oxytocin levels, making them feel better. Singing can also help reduce anxiety and fear, as it distracts the mind and provides a sense of freedom.
Physically, singing can have a positive impact on the body. It can increase lung capacity and improve breathing, which can help in managing symptoms of anxiety and panic. Singing can also stimulate the release of endorphins, which are natural pain relievers, providing a sense of relief and relaxation.
Additionally, singing can be a great way to connect with others and build a support community. Joining a choir or singing group can provide a sense of belonging and offer opportunities for social interaction. It can also help reduce feelings of isolation and loneliness that often accompany postpartum depression.
If you’re not comfortable singing in a group setting, you can still benefit from singing alone. Singing along to your favorite songs or watching a music video can provide a much-needed distraction and boost your mood. It can also serve as a form of self-expression and help process emotions related to postpartum depression.
Remember, it’s important to seek professional help if you’re experiencing postpartum depression. A therapist or healthcare provider can discuss your symptoms and help develop a treatment plan that may include psychotherapy, medications, or other services. Singing can be used as a complementary tool to enhance your overall well-being.
In conclusion, singing can be a valuable and effective strategy for coping with postpartum depression. It can help improve mood, reduce anxiety, and promote a sense of connection and community. So why not give it a try? Singing just might be the free, accessible, and enjoyable tool that helps you feel better.
Postpartum Depression
Postpartum depression is a common mental health disorder that affects new mothers. It is estimated that about one in every four women will experience some form of postpartum depression. The condition can have a significant impact on a woman’s well-being, relationships, and ability to care for her newborn.
Doctors and healthcare providers recommend seeking help and advice if you are feeling overwhelmed or experiencing symptoms of postpartum depression. It is important to remember that you are not alone and there are resources available to support you.
If you are suffering from postpartum depression, it is important to talk to your healthcare provider, such as your pediatrician, who can help you navigate through the different treatments and resources available. They can provide guidance on managing stress, improving your mental health, and ensuring the safety of your newborn.
One treatment option that is gaining popularity is brexanolone, a medication that has shown promise in reducing the symptoms of postpartum depression. However, this treatment may not be suitable for everyone, and it is important to discuss the risks and benefits with your healthcare provider.
In addition to seeking medical advice, there are some self-help tips that can help improve your mental health during this challenging time. It is important to take breaks and prioritize self-care, even if it means asking for help with household errands or childcare. Joining support groups or talking to a counselor can also be beneficial in reducing feelings of loneliness and isolation.
It is crucial to have open and honest communication with your partner. They can provide support and understanding, and together you can work towards improving your mental health. It is also important to set realistic expectations for yourself and not to put too much pressure on being a “perfect” parent.
It is important to remember that postpartum depression is a temporary condition and with the right support and treatment, it can improve. However, if your symptoms persist or worsen, it is important to seek professional help. Your healthcare provider can recommend further treatments or refer you to a specialist who can provide the necessary support.
Postpartum depression can have lasting effects on your mental health and relationships, but with proper support and treatment, you can overcome this challenging time and bond with your child in a healthy and loving way.
Overview
Postpartum depression is a condition that affects many women after childbirth. It is a mental health disorder that can have physical, emotional, and psychological consequences. Women with postpartum depression often experience feelings of sadness, emptiness, and exhaustion. They may have trouble bonding with their baby and may feel guilty about not enjoying motherhood as much as they expected.
Postpartum depression is often caused by a combination of factors, including hormonal changes, a history of depression or anxiety, a difficult or traumatic childbirth, and lack of support from loved ones or friends. It can also be influenced by external factors such as stress, lack of sleep, and changes in routine and responsibilities.
Signs and symptoms of postpartum depression may include feelings of sadness, hopelessness, and worthlessness, changes in appetite and sleep patterns, loss of interest in activities previously enjoyed, difficulty concentrating, and increased irritability or frustration. Some women may also experience physical symptoms such as headaches, stomachaches, or chest pain.
If you think you may be experiencing postpartum depression, it is important to talk to your healthcare provider. They can help you establish a diagnosis and develop a treatment plan that is safe for you and your baby. Treatment options may include therapy, medication, or a combination of both. Some women find that talking to a therapist or joining a support group can be helpful in managing their symptoms.
There are also self-care strategies that can help improve symptoms of postpartum depression. These may include getting enough rest, eating a balanced diet, exercising regularly, and asking for help when needed. It is important to prioritize self-care and take time for yourself, even if it feels difficult or selfish.
It is also important to reach out for support. Friends, family, and other loved ones can be a source of understanding and comfort during this challenging time. There are also many resources available, including international helpline services and postpartum depression support centers, that can provide guidance and assistance.
Postpartum depression is a real and serious condition. It is not a sign of weakness or failure as a mother. Many women experience postpartum depression, and it is important to remember that you are not alone. With the right support and treatment, you can recover and enjoy your time with your baby.
| Fact: | Postpartum depression can happen to anyone, including women who have had a healthy pregnancy, a positive birth experience, or who have had no history of depression before. |
| Fact: | Postpartum depression can develop anytime within the first year after giving birth, although it is most commonly experienced within the first three months. |
| Fact: | Postpartum depression is different from the “baby blues,” which is a temporary condition that affects many women in the first few weeks after childbirth. The baby blues usually go away on their own within a few days or weeks. |
| Fact: | There is a medication called brexanolone that has been approved by the U.S. Food and Drug Administration for the treatment of postpartum depression. It is administered in a hospital setting and has been shown to be effective in reducing symptoms. |
What is postpartum depression
Postpartum depression, also known as PPD, is a condition that affects some mothers after giving birth. It is estimated that around 15% of women experience postpartum depression, although the actual number of cases may be higher due to underreporting.
Postpartum depression is characterized by feelings of extreme sadness, anxiety, and fatigue that can interfere with a mother’s ability to care for herself and her baby. These emotions can range from mild to severe and may last for several weeks or even months if left untreated.
The exact cause of postpartum depression is not known, but it is believed to be a combination of hormonal, psychological, and environmental factors. The sudden drop in hormone levels, particularly estrogen and progesterone, after childbirth is thought to contribute to the development of postpartum depression. Other factors such as sleep deprivation, stress, and changes in lifestyle and relationships can also increase the risk.
Signs and symptoms of postpartum depression can vary from person to person but may include:
- Feeling overwhelmed and unable to cope
- Intense mood swings
- Loss of interest in activities once enjoyed
- Difficulty bonding with the baby
- Excessive crying or irritability
- Extreme fatigue or lack of energy
- Changes in appetite and sleep patterns
- Feelings of guilt or worthlessness
- Thoughts of harming yourself or the baby
If you or someone you know is experiencing these signs and symptoms, it is important to seek help from a healthcare professional. Postpartum depression can be treated and early intervention can improve the outcome for both the mother and the baby.
Treatment options for postpartum depression may include therapy, medication, and support groups. Cognitive-behavioral therapy can help mothers manage their thoughts and emotions and develop healthy coping strategies. Medications such as antidepressants may be prescribed to help balance the chemical imbalances in the brain. Support groups offer a safe space for mothers to share their experiences and gain support from others who are going through similar challenges.
In some cases, more intensive treatment may be needed. For example, a medication called brexanolone has been approved by the FDA for the treatment of postpartum depression. This medication is administered through an intravenous infusion and can help improve symptoms within a few days.
It is important to remember that postpartum depression is a medical condition and not a sign of weakness or personal failure. It is also important to note that postpartum depression can affect anyone, regardless of their socioeconomic status or personal circumstances.
If you or someone you know is struggling with postpartum depression, reach out for help. Talk to a healthcare professional, join a support group, and lean on friends and family for support. Remember that you are not alone, and with the right treatment, you can overcome postpartum depression and start enjoying the special moments of motherhood.
What are the types of postpartum depression
Postpartum depression is a common condition that affects many new mothers. It can have various types and levels of severity. Understanding these types can help individuals recognize the signs and seek appropriate treatment.
- Postpartum blues: This is a milder and more common type of postpartum depression. It usually occurs within the first week after childbirth and may involve frequent mood swings, irritability, fatigue, and tearfulness. These symptoms generally improve on their own without medical intervention.
- Postpartum depression (PPD): PPD is a more severe and long-lasting condition. It can develop within the first few weeks after childbirth and may last for several months. Symptoms include sadness, anxiety, loss of interest in activities, changes in appetite and sleep patterns, difficulty bonding with the baby, and feelings of worthlessness or guilt.
- Postpartum anxiety disorder: Some individuals may experience intense anxiety after giving birth. This type of postpartum depression can manifest as constant worry, panic attacks, restlessness, and an overwhelming fear that something bad will happen to their baby.
- Postpartum obsessive-compulsive disorder (OCD): OCD involves intrusive thoughts and compulsive behaviors that can interfere with daily life. New mothers with postpartum OCD may experience repeated and unwanted thoughts of harming the baby or themselves, and engage in rituals or behaviors to neutralize these thoughts.
- Postpartum post-traumatic stress disorder (PTSD): This type of postpartum depression is triggered by a traumatic childbirth experience. Women with postpartum PTSD may have flashbacks, nightmares, and emotional distress related to the event. They may also avoid reminders or discussions about childbirth.
- Postpartum psychosis: Postpartum psychosis is a rare but severe condition that requires immediate medical attention. Symptoms include confusion, hallucinations, delusions, disorganized behavior, and thoughts of harming oneself or the baby. Hospitalization may be necessary to ensure the safety of the mother and child.
It’s important to remember that postpartum depression can affect anyone and that seeking help is crucial for the well-being of both the mother and the child. If you or someone you know experiences any of these types of postpartum depression, it is essential to discuss it with a physician or mental health professional to determine the most appropriate course of action.
Treatment options for postpartum depression vary and may involve therapy, medication, or a combination of both. In some cases, additional support from friends, family, or support groups can be helpful in overcoming the challenges of postpartum depression.
It’s also important to establish a strong support system and take care of oneself physically and emotionally. Strategies such as getting enough rest, eating a balanced diet, and engaging in regular exercise can make a significant difference in one’s well-being.
Researchers are constantly working to develop new and effective treatments for postpartum depression. One example is brexanolone, an intravenous medicine that has shown promise in treating severe PPD. Other emerging treatments focus on harnessing the effects of oxytocin to enhance maternal-infant attachment and well-being.
In conclusion, postpartum depression can take different forms and levels of severity. Recognizing the signs, seeking support, and discussing treatment options with a healthcare professional are crucial steps in overcoming the challenges of postpartum depression.
Who is affected by postpartum depression
Postpartum depression (PPD) is a common condition that affects many new mothers. It is estimated that up to one in seven women may experience PPD after giving birth. PPD can occur in women of all ages and backgrounds, though it is more common in women who have a history of depression or anxiety.
PPD can also affect fathers and partners, though the prevalence is lower compared to mothers. Research shows that between 4% and 25% of fathers experience symptoms of postpartum depression. Fathers who have a history of depression or whose partners are suffering from PPD are more likely to be affected.
It is important to note that PPD is not a sign of weakness or a lack of love for your child. It is a medical condition that can make it harder for you to take care of yourself and your baby. PPD is often characterized by feelings of sadness, anxiety, and worthlessness. Many new parents may also experience mood swings and have trouble sleeping.
PPD can have a significant impact on a person’s ability to function in their daily life. It may affect their ability to take care of their child, perform tasks at work, and maintain relationships. If left untreated, PPD can persist for several months or even longer.
If you suspect that you or someone you know may be suffering from PPD, it is important to seek help. Talk to your healthcare provider, such as your OB/GYN or primary care doctor, who can provide a diagnosis and recommend appropriate treatments. Remember, you are not alone, and there are many resources available to help you through this challenging time.
The first step to getting help is reaching out. There are many support groups and community organizations that provide a lifeline to those suffering from PPD. These groups can provide a safe space to discuss your feelings and experiences with others who are going through the same thing. It can be a great way to find comfort, share coping strategies, and gain insight into treatments that have worked for others.
Beyond support groups, there are also various treatments available for PPD. These can range from therapy and counseling to medication, depending on the severity of symptoms. Your healthcare provider will work with you to develop a treatment plan that is right for you.
Remember that it takes time for PPD to develop and that it is not your fault. Give yourself permission to seek help and take care of yourself. Be patient and kind to yourself, and don’t wait for things to get worse before seeking help.
If you are feeling overwhelmed, scared, or unable to cope, don’t hesitate to make an appointment with your healthcare provider. They are there to support you and provide the care you need. You should never feel alone or helpless.
In conjunction with professional help, there are also several things you can do at home to help manage PPD. It is important to take care of yourself physically and emotionally. Make time for self-care activities that you enjoy, such as taking walks, reading, or practicing mindfulness. Reach out to loved ones for support, and consider asking for help with tasks like cooking, cleaning, or diapers.
Remember that PPD is a temporary condition, and with the right support and treatment, you will recover. It is important to be patient with yourself and to give yourself credit for the small victories along the way. You are stronger than you think, and you will get through this.
How do I know if I have baby blues or postpartum depression
Mentally, the disorders of baby blues and postpartum depression can look very similar. It’s important to recognize the signs and seek help if you’re struggling. While most women experience a mild form of the baby blues after giving birth, postpartum depression is a more serious condition that can have long-term effects on your mental health. Here are some key differences to look out for:
Baby Blues:
The baby blues are a common experience for many women after giving birth. It is usually a short-lived period of mild mood swings, irritability, sadness, and anxiety. These feelings may come and go throughout the day and can be overwhelming at times. Typically, baby blues occur in the first two weeks after childbirth and tend to resolve on their own without treatment.
Postpartum Depression:
Postpartum depression, on the other hand, lasts longer and can have a more significant impact on a woman’s ability to function. If you feel persistently sad, hopeless, or overwhelmed for more than two weeks after giving birth, you may be experiencing postpartum depression. Other symptoms include changes in appetite and eating habits, difficulty sleeping or sleeping too much, loss of interest in activities you once enjoyed, trouble bonding with your baby, feeling excessively tired, having extreme mood swings, and having thoughts of self-harm or harming your baby.
If you recognize these symptoms in yourself or a loved one, it’s important to seek help from healthcare providers who specialize in postpartum depression. They can discuss treatment options, including therapy, medication, and self-care strategies, to help you find a balance and overcome your symptoms. Remember, you are not alone. Postpartum depression is a common condition, and there are resources available to support you throughout your journey.
How long does postpartum depression last
Postpartum depression is a condition that affects new mothers and typically occurs within the first few weeks after childbirth. However, it is important to note that the duration of postpartum depression can vary among women. For some women, it may only last a few weeks or months, while for others, it may persist for a year or more.
Postpartum depression is characterized by feelings of sadness, hopelessness, and a lack of interest in activities that were once enjoyed. It can also include difficulty sleeping, changes in appetite, and trouble concentrating. The hormonal changes that occur in a woman’s body after birth, including a decrease in levels of oxytocin, often referred to as the “love hormone,” can contribute to the development of postpartum depression.
During the postpartum period, a woman’s brain undergoes significant changes. The arrival of a newborn triggers a cascade of hormonal fluctuations and adjustments, which can affect a woman’s emotional well-being. Additionally, the intense physical and emotional demands of caring for a newborn, coupled with sleep deprivation and the potential loss of independence, can contribute to feelings of overwhelm and stress.
If you suspect that you or a loved one may be experiencing postpartum depression, it is important to seek help from a healthcare professional, such as an OBGYN or a nurse in the postpartum department. They can administer a test to assess the severity of the depression and recommend appropriate treatment options.
Treatment for postpartum depression may include counseling, therapy, and, in more severe cases, medication. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) can be helpful in balancing mood and improving overall well-being. It may take several weeks for the medication to take effect, so it is important to be patient and continue with the prescribed treatment.
In addition to seeking professional help, there are also several self-care practices that may be useful in managing postpartum depression. These include getting enough rest, engaging in activities that bring joy and relaxation, connecting with other new mothers for support, and practicing techniques such as meditation or deep breathing exercises to reduce stress.
It is also important to manage expectations and be realistic about the challenges of the postpartum period. Remember that it is normal to feel overwhelmed and it is okay to ask for help. Reach out to your partner, family, or friends for assistance with childcare or other responsibilities, so that you can take time for self-care and focus on your well-being.
For non-birthing partners, it is important to be understanding and supportive. Postpartum depression can affect anyone caring for a newborn, regardless of gender. Offering a listening ear, providing assistance with household chores, and encouraging open communication can go a long way in helping your loved one navigate through this challenging time.
If you or someone you know is experiencing signs of postpartum depression, such as persistent feelings of sadness, hopelessness, or a loss of interest in daily activities, it is important to seek help as soon as possible. Postpartum depression should not be ignored, as it can have serious implications for both the mother’s mental well-being as well as the overall family dynamic.
| Common signs and symptoms of postpartum depression: |
|---|
| – Persistent feelings of sadness or hopelessness |
| – Loss of interest in activities once enjoyed |
| – Difficulty sleeping or changes in sleep patterns |
| – Changes in appetite or weight |
| – Fatigue and lack of energy |
| – Trouble concentrating or making decisions |
| – Feelings of guilt or worthlessness |
| – Thoughts of death or suicide |
If you or someone you know is experiencing any of these symptoms, it is important to reach out for help. Postpartum depression is a treatable condition, and with the right support and treatment, it is possible to recover and enjoy the journey of motherhood.
What factors increase my risk of being depressed after the birth of my child
Postpartum depression is a common condition that affects many women after childbirth. While the exact cause is unknown, there are several factors that can increase the risk of developing this condition. Understanding these risk factors can help you be more prepared and seek the necessary support if needed.
One factor that can contribute to postpartum depression is the hormonal changes that occur after giving birth. The sudden drop in hormones such as estrogen and progesterone can affect a woman’s mood and increase the likelihood of experiencing depression. Sleep deprivation is another common factor that can worsen a new mother’s mood. The demands of caring for a newborn can result in a lack of sleep, which can further increase the risk of depression.
Another important factor is a history of depression or previous episodes of postpartum depression. If you have experienced depression in the past, you are more likely to face it again after childbirth. Additionally, a lack of support from loved ones or strained relationships can contribute to feeling overwhelmed and increase the risk of depression. Lack of social support may also impact bonding with the newborn.
Feeling overwhelmed by the task of caring for a newborn and adjusting to different routines and responsibilities can also increase the risk of postpartum depression. It is important to understand that these feelings are common and reaching out for help is not a sign of weakness, but a necessary step to improve your well-being and the well-being of your child.
Other factors that can contribute to postpartum depression include a difficult or traumatic childbirth experience, financial stress, and a lack of resources. It is also important to note that postpartum depression can affect any woman, regardless of age, race, or socioeconomic status.
If you are experiencing any symptoms of postpartum depression, such as a persistent feeling of sadness or emptiness, loss of interest in activities you once enjoyed, difficulty sleeping or sleeping too much, changes in appetite, feelings of guilt or worthlessness, or thoughts of self-harm or harming the baby, it is important to seek immediate help.
Remember, postpartum depression is a treatable condition, and with the right support and treatment, you can recover and enjoy the joys of motherhood. Speaking to healthcare professionals, joining support groups, or seeking therapy can provide the necessary tools to cope with postpartum depression and improve your overall well-being.
Here are some additional tips that can help improve your mood and well-being as a new mother:
- Make sure to get enough sleep whenever possible. Nap when your baby sleeps and ask for help with nighttime feedings.
- Reach out for support from loved ones, friends, or support groups who can provide emotional and practical assistance.
- Take time for self-care. Engage in activities or hobbies you enjoy, even if it’s just for a few minutes a day.
- Practice relaxation techniques such as deep breathing or meditation to help manage stress.
- Get outside and spend time in nature. Being in green spaces can have a positive impact on your mood.
- Talk openly about your feelings and experiences with trusted individuals or healthcare professionals who can offer guidance and support.
It is crucial to remember that postpartum depression is a temporary condition and with the right support and treatment, you can overcome it. Seek help and take the necessary steps to prioritize your mental health as you navigate this new chapter of your life.
Symptoms and Causes
Postpartum depression is a type of mood disorder that often occurs after the birth of a baby. It is important to know the symptoms and causes of this condition to better understand and address it.
Some common symptoms of postpartum depression include feeling sad, hopeless, and moody. You may also experience a lack of interest or pleasure in activities you once enjoyed. Other symptoms can include changes in appetite or eating habits, trouble sleeping or sleeping too much, feeling overwhelmed or worthless, and having thoughts of harming yourself or your baby.
The exact causes of postpartum depression are not known, but it is believed to be a combination of physical, emotional, and environmental factors. Hormonal changes that occur after childbirth, such as a drop in reproductive hormones like estrogen and progesterone, may play a role in the development of postpartum depression. Other factors that can contribute to the condition include a history of depression or anxiety, a lack of social support, and experiencing a difficult or traumatic childbirth.
It is important to seek help if you think you may have postpartum depression. Many resources are available to help new mothers, including support groups, counseling services, and medical professionals. Treatment options for postpartum depression may include therapy, medication, or a combination of both.
Preventive measures can also be taken to reduce the risk of developing postpartum depression. Taking good care of yourself throughout your pregnancy and after the arrival of your baby is essential. This includes getting enough rest, eating a healthy diet, and staying active. It is also important to reach out for support from loved ones, friends, and healthcare providers. Remember that you are not alone, and seeking help is the best thing you can do for yourself and your baby.
Postpartum depression is not something to be taken lightly. It is a serious condition that can have a significant impact on a person’s life. If you or someone you know is experiencing symptoms of postpartum depression, it is important to reach out for help. Remember that there are resources available and treatments that can help you find relief.
- Cleveland Clinic’s Marilyn Calverley Department of Obstetrics and Gynecology offers comprehensive care for women experiencing postpartum depression. They provide a range of resources and treatment options to support women throughout their journey.
- It is important to remember that postpartum depression can be a temporary condition and with the right support and treatment, many women are able to overcome it and go on to lead happy, healthy lives.
- If you or someone you know is struggling with postpartum depression, don’t hesitate to reach out for help. You are not alone, and there are people who can help you through this challenging time.
Remember, postpartum depression is a real and treatable condition. It is important to prioritize your mental health and seek the support and care you need. Don’t be afraid to ask for help, and remember that you are not alone in this journey.
What are the symptoms of postpartum depression
Postpartum depression (PPD) is a common condition that affects many new mothers. It is important to be aware of the signs and symptoms, as early detection and treatment can lead to improved outcomes for both the mother and baby.
One common symptom of postpartum depression is a feeling of extreme sadness or low mood. This can include crying spells, feeling overwhelmed or hopeless, and a loss of interest in activities that used to bring joy. Another symptom is a persistent feeling of anxiety or worry. Some mothers may experience physical symptoms such as headaches, stomachaches, or changes in appetite and sleep patterns. They might also have trouble concentrating or making decisions.
Many women with PPD may have difficulty bonding with their baby. They may feel detached or have thoughts that they are not a good mother. Some women may feel guilty for not enjoying motherhood or may have thoughts of harming themselves or their baby. These are serious symptoms and it is important to seek help right away.
Some women with PPD may also experience feelings of anger or irritability. They may feel easily overwhelmed and lash out at their partners or loved ones. This can strain relationships and make it even harder for them to seek help.
It is important to note that not all women will experience the same symptoms. PPD can present differently for different individuals. Some women may have mild symptoms that come and go, while others may have severe symptoms that interfere with their daily functioning.
If you or someone you know is experiencing symptoms of postpartum depression, it is important to reach out for help. Doctors, nurses, and other healthcare providers can provide guidance and recommend treatment options. Options for treatment may include therapy, support groups, medication, or a combination of these approaches.
Support and understanding from loved ones is also crucial. Encouraging new mothers to take care of themselves, engaging in activities they enjoy, and offering help with tasks like diaper changes or babysitting can make a big difference. Perinatal support centers and helplines are available to provide information, resources, and a listening ear for those in need.
Remember, postpartum depression is a medical condition and should be treated as such. It is not a sign of weakness or a failure to be a good mother. With the right support and treatment, many women are able to recover and thrive during this challenging time.
What causes postpartum depression
Postpartum depression (PPD) is a serious depressive disorder that affects mothers who have recently given birth. It is not the same as the “baby blues,” which are temporary mood swings that many women experience after childbirth.
PPD can occur within the first few weeks after delivery, but it can also develop later, up to six months after giving birth. The exact cause of PPD is not known, but it is believed to be a combination of biological, psychological, and social factors.
Some common factors that can contribute to the development of PPD include:
- Hormonal changes: After childbirth, there is a rapid drop in the levels of hormones, such as estrogen and progesterone, which can affect the mood and emotions of a new mother.
- History of mental health disorders: Women with a history of depression, anxiety disorders, or other mental health conditions are more likely to develop PPD.
- Stress and lack of support: The stress of taking care of a newborn, combined with the lack of emotional and practical support from loved ones, can increase the risk of PPD.
- Psychological factors: Women who have negative thoughts and beliefs about themselves, their abilities as mothers, or their relationship with their baby are more prone to developing PPD.
- Previous experience of PPD: Women who have previously experienced PPD are at a higher risk of developing it again in subsequent pregnancies.
If you are experiencing symptoms of PPD, it is important to seek help and support. You can start by speaking with your healthcare provider, such as your obstetrician/gynecologist (OBGYN) or a mental health professional. They can recommend different treatment options, such as therapy, support groups, or, in some cases, antidepressant medication.
Some strategies that may help manage and decrease the symptoms of PPD include:
- Getting enough rest and sleep, even if it means asking for help with the baby.
- Eating a nutritious diet, as certain nutrients can contribute to overall well-being and mood.
- Engaging in physical activity or exercise, as it can boost mood and reduce stress.
- Taking breaks and doing activities that you enjoy, even if it’s just for a short period of time.
- Seeking emotional support from loved ones, friends, or support groups.
- Considering additional support services, such as postnatal care centers or educational resources.
If you’re worried about yourself or someone you know, and you suspect PPD, it’s important to encourage them to seek care and support. Early diagnosis and intervention can help improve the prognosis and reduce the impact of this condition on the mother’s overall well-being and the newborn’s development.
Remember, postpartum depression is a psychological disorder that requires professional evaluation and treatment. Don’t hesitate to reach out for help if you’re experiencing the symptoms or are concerned about someone you care about.
Can postpartum depression affect my baby
Postpartum depression is a condition that can affect new mothers, and it is important to recognize that it can also have an impact on their babies. It is a common misconception that only mothers experience postpartum depression, but the reality is that it can extend to the baby as well.
Babies can pick up on their mother’s emotions and feelings. When a mother is experiencing postpartum depression, she may have difficulty bonding with her baby and providing the care and attention that a newborn needs. This can lead to difficulties in the baby’s development and overall well-being.
Research has found that when a mother experiences postpartum depression, her baby is more likely to have limited social interactions, developmental delays, and behavioral problems. The baby may have difficulty forming healthy relationships and may have increased risk of emotional and psychological issues later in life.
It is important for mothers to understand that postpartum depression can have a significant impact on their child. The good news is that there are preventive measures and resources available to help both the mother and the baby. Seeking professional help and talking to a healthcare provider or a certified therapist is a good step towards recognizing and dealing with postpartum depression.
Mothers should also take care of themselves by getting enough rest, eating well, and finding ways to relax and enjoy their time with their baby. Support from family, friends, and the community can also be valuable in helping mothers cope with postpartum depression.
Motherhood can be challenging, and it is important to give yourself permission to ask for help. Recognize the signs of postpartum depression, such as feelings of sadness, hopelessness, and the inability to enjoy things that used to bring you pleasure. Know that you are not alone, and there are resources available to help you through this difficult time.
Remember that seeking help is a sign of strength, and it is in the best interest of both you and your baby. With the right support, you can overcome postpartum depression and provide your baby with the care and love they need.
Postpartum depression can be a temporary condition, but it is important to understand that it can also last for longer periods. The severity and duration of postpartum depression can vary from person to person, but it is essential to take it seriously and seek help when needed.
If you or someone you know is experiencing postpartum depression, reach out to a healthcare provider or a certified therapist. They can provide the guidance, support, and treatment options that can decrease the symptoms and help you feel better.
Remember, taking care of yourself is an essential part of taking care of your baby. You are not alone, and there is hope. Reach out, ask for help, and know that you can overcome postpartum depression.
Diagnosis and Tests
Postpartum depression (PPD) is a common condition that affects many new mothers. It is important to be aware of the symptoms and to seek help if you think you may be experiencing PPD. Diagnosis of postpartum depression usually requires a thorough assessment by a healthcare professional.
If you are experiencing symptoms such as persistent feelings of sadness, hopelessness, or being overwhelmed, it is important to reach out for support. Your healthcare provider may ask you questions about your mood, appetite, sleep patterns, and overall well-being. They may also ask about your experiences with bonding and parenting, as well as your thoughts on food and eating.
It is important to note that postpartum depression is often underdiagnosed and undertreated. Many women fear being judged or labeled as a bad mother, which prevents them from seeking help. However, there are several diagnostic tools available to healthcare professionals to assess and diagnose PPD.
One common tool used is the Edinburgh Postnatal Depression Scale (EPDS). This self-report questionnaire consists of 10 questions that can help identify symptoms of depression. It is often administered during a routine postpartum check-up with a healthcare provider.
In addition to the EPDS, other tests may be used, such as the Postpartum Depression Screening Scale (PDSS) or the Beck Depression Inventory (BDI), depending on the healthcare provider’s preference.
It is important to remember that a diagnosis of postpartum depression does not necessarily mean that you will require medication. In mild cases, self-help strategies, counseling, and support groups may be recommended. However, in more severe cases of PPD, medication such as antidepressants may be prescribed. Some medications, like brexanolone, have been specifically developed for the treatment of PPD and have shown promising results.
It is essential to consult with a healthcare provider before starting any medication, especially if you are breastfeeding. They can provide guidance on the best treatment options for you and your baby’s well-being.
Therapy, both individual and group, can also be effective in treating PPD. Cognitive-behavioral therapy (CBT), which focuses on changing negative thought patterns and behaviors, has been shown to help many women with PPD.
In some cases, a healthcare provider may recommend a combination of medication and therapy for optimal management of PPD.
It is also important to engage in self-care activities to promote overall well-being. This can include getting enough rest, eating nutritious food, and seeking support from loved ones. Taking time for yourself, even if it’s just a few minutes each day, can help alleviate some of the stress and exhaustion that comes with caring for a newborn.
If you suspect that you or someone you know may be experiencing postpartum depression, it is important to seek help as soon as possible. This could involve making an appointment with a healthcare provider, reaching out to a counselor, or calling a helpline. Remember, PPD is a common condition and you are not alone.
How is postpartum depression diagnosed
Postpartum depression (PPD) is a serious condition that affects many new mothers. It is essential to trust your instincts and seek help if you suspect you may be experiencing PPD. Diagnosing PPD involves a careful evaluation by a healthcare professional.
Mild episodes of postpartum depression can be similar to the “baby blues,” which many women experience after giving birth. These feelings of sadness, mood swings, and anxiety are normal after childbirth and usually resolve on their own within a few weeks. However, if these symptoms persist and become more severe, it may be a sign of postpartum depression.
Healthcare professionals, such as pediatricians or family doctors, can recognize and diagnose postpartum depression. They will evaluate the mother’s symptoms and may ask questions about her feelings, sleeping patterns, appetite, and ability to care for herself and her baby. They may also consider other factors that affect mental health, such as a history of depression, anxiety, or trauma.
In some cases, a healthcare provider may recommend screening tools, such as questionnaires or behavioral assessments, to help assess the severity of the depression. These assessments can help identify the level of risk and guide treatment recommendations.
The healthcare provider takes into account the specific needs of the mother and the baby, as postpartum depression can also affect the child’s well-being. In cases where the child’s safety is a concern, a healthcare provider may recommend hospitalization or additional support services.
A warm and supportive environment is crucial during the diagnosis process. The healthcare provider should engage in a non-judgmental conversation with the mother, providing emotional support and reassurance. They should let the mother know that she is not alone and that postpartum depression is a common condition that can be managed with the right treatment and support.
In some cases, additional assessments or referrals to mental health professionals may be needed to confirm the diagnosis or provide specialized care. The healthcare provider might also recommend lifestyle adjustments, such as getting more rest, adjusting nutrient intake, or engaging in hobbies and self-care activities.
It is important for the mother to recognize that seeking help is not a sign of weakness or failure. Postpartum depression is a medical condition that requires treatment and support. With the right care, mothers affected by postpartum depression can recover and have a healthy, fulfilling relationship with their child.
It is worth mentioning that there are medications available to treat postpartum depression, such as brexanolone. However, the use of medication should be carefully considered, weighing the potential risks and benefits, and should be done under the guidance of a healthcare professional.
How do doctors screen for postpartum depression
Postpartum depression (PPD) is a common condition that affects many new mothers. It is important for doctors to screen for PPD to ensure that new mothers receive the support and treatment they need. Here are some ways doctors may screen for postpartum depression:
- Questionnaires: Doctors may ask new mothers to complete questionnaires that assess their mood and feelings. These questionnaires are designed to identify symptoms of PPD, including feelings of sadness, irritability, and loss of interest.
- Conversation: Doctors will often have conversations with new mothers to discuss their experiences and emotions. They may ask about changes in mood, sleeping patterns, and appetite to help identify possible signs of PPD.
- Monitoring: Doctors may monitor changes in a new mother’s behavior, such as sudden mood swings or a drop in energy levels. They may also pay attention to any sudden changes in the mother’s interactions with her baby or other family members.
- Additional assessments: In some cases, doctors may recommend additional assessments, such as blood tests or hormone level checks, to rule out any other medical conditions that may be contributing to the symptoms of PPD.
- Advice on coping strategies: Doctors may provide advice on coping strategies and self-care techniques that new mothers can use to manage and reduce symptoms of PPD. This may include recommendations for rest, exercise, seeking support from loved ones, and engaging in activities that promote relaxation and well-being.
- Referral: In severe cases, doctors may refer new mothers to specialized mental health professionals, such as licensed therapists or psychiatrists, who can provide additional support and treatment for PPD.
It is important for doctors to screen for postpartum depression because it can have a significant impact on a mother’s well-being and her ability to care for her baby. By identifying and addressing PPD early on, doctors can help ensure that mothers receive the necessary support and treatment to navigate this challenging period of motherhood.
Management and Treatment
Management of postpartum depression involves a combination of different approaches and interventions. It is important to remember that every woman’s experience with postpartum depression is unique, so treatment may vary from person to person. Here are some tips and suggestions for managing and treating postpartum depression:
1. Seek professional help: If you are experiencing symptoms of postpartum depression, it is important to reach out to a healthcare professional. They can provide you with the necessary support and guidance to help you navigate through this challenging period. Your healthcare provider may conduct tests to establish a diagnosis and recommend a suitable treatment plan.
2. Talk to others: Sharing your feelings and experiences with trusted friends, family, or support groups can be helpful in reducing feelings of loneliness and increasing social support. It can also provide you with a safe space to express your emotions and concerns.
3. Take care of your physical health: Eating a healthy diet and engaging in regular physical activity can help improve your mood and overall well-being. Make sure to establish a routine and prioritize self-care activities that you enjoyed before having a baby.
4. Consider therapy: Psychotherapy, such as cognitive-behavioral therapy (CBT), can be an effective treatment option for postpartum depression. It can help you identify and change negative thought patterns and develop healthy coping mechanisms.
5. Antidepressant medication: In some cases, healthcare providers may prescribe antidepressant medication to help alleviate symptoms of postpartum depression. Selective serotonin reuptake inhibitors (SSRIs) are commonly used antidepressants that can help regulate mood levels. It is important to consult with your healthcare provider to determine if medication is necessary and safe for you.
6. Get enough sleep: Lack of sleep can contribute to mood swings and exacerbate symptoms of postpartum depression. Try to establish a sleep routine and ask for help from your partner or other family members in caring for the baby, so you can get enough rest.
7. Bonding with your baby: Building a strong bond with your baby can be a great source of joy and fulfillment. Spend quality time with your baby, engage in activities such as cuddling, playing, and talking to them. This can help increase feelings of connection and reduce feelings of isolation.
8. Be aware of symptoms of postpartum psychosis: Postpartum psychosis is a rare but serious condition that involves a significant change in mood and behavior. If you experience frequent crying, delusions, hallucinations, or thoughts of harming yourself or your baby, seek emergency medical care immediately.
9. Don’t be too hard on yourself: Remember that postpartum depression is not your fault, and you are not alone. It is a common condition that can happen to anyone. Be compassionate with yourself and seek support from loved ones.
10. Hope for the future: While postpartum depression can feel overwhelming, it is important to remember that with proper treatment and support, it is a treatable condition. With time, the symptoms can decrease and improve your quality of life. Have faith in the healing process and believe that things will get better.
In summary, management and treatment of postpartum depression involve seeking professional help, talking to others, taking care of your physical health, considering therapy or antidepressant medication, getting enough sleep, bonding with your baby, being aware of symptoms of postpartum psychosis, and being compassionate with yourself. Remember, there is hope, and you are not alone in this journey.
How is postpartum depression treated
Postpartum depression is a serious condition that affects many new mothers. It is important to seek help and treatment if you or someone you know is experiencing symptoms of postpartum depression. There are several treatment options available that can help alleviate the symptoms and improve the well-being of the mother and her family.
One of the most important aspects of treatment for postpartum depression is building trust with a healthcare provider. The mother needs to feel comfortable and supported by her provider in order to open up about her feelings and receive the necessary help. It is not the mother’s fault that she is experiencing this condition, and it is important for her to understand that.
Treatment for postpartum depression can involve several different forms. Cognitive-behavioral therapy (CBT) is a common approach that involves counseling sessions to help the mother identify and change negative thought patterns. This can be a great tool for learning to manage the symptoms and develop healthy coping strategies.
In more severe cases, antidepressant medication may be prescribed. These medications can help regulate the mother’s mood and alleviate some of the symptoms of postpartum depression. However, it is important to weigh the risks and benefits of medication, as there can be side effects and concerns about the safety of the baby if the mother is breastfeeding.
In addition to therapy and medication, there are also lifestyle changes that can be helpful in treating postpartum depression. Getting enough sleep, eating a healthy diet, and engaging in regular exercise can all contribute to improved emotional well-being. It is also important for the mother to carve out time for herself and engage in activities that she enjoys.
Support from family and friends is crucial during this time. Loved ones can help with tasks such as diaper changing and feeding, allowing the mother to get much-needed rest. It is also important for the mother to reach out for help and not try to do everything on her own.
For those suffering from postpartum depression, it is common to feel panicked, scared, hopeless, and overwhelmed. It is important to remember that these symptoms are temporary and can be treated. By seeking help and treatment, the mother can learn to manage her emotions and develop a strong bond with her baby.
It is also important to recognize that postpartum depression can affect anyone. It is not limited to first-time mothers, and can occur in those who have had multiple children. The risk for developing postpartum depression is higher for those who have a history of depression, anxiety, or other mental health disorders.
If you or someone you know is experiencing symptoms of postpartum depression, do not hesitate to seek help. Early intervention can lead to better outcomes for both the mother and her baby. Remember, you are not alone, and there are resources available to support you through this challenging time.
What medications can I take for postpartum depression
If you’re experiencing postpartum depression, it’s important to seek help and explore different treatment options. While counseling and support from friends and family can be beneficial, some women may require medication to help manage their symptoms. Medication can be particularly helpful if you’ve been experiencing severe or frequent symptoms that affect your ability to care for yourself or your newborn.
Talking to a medical professional, such as your OB-GYN, can help you determine the best course of action. They can evaluate your condition and diagnose postpartum depression. After a thorough examination, they may recommend medication as part of your treatment plan.
There are several medications that can be used to manage postpartum depression, including antidepressants, anti-anxiety medications, and mood stabilizers. These medications work by targeting the hormone imbalances that contribute to the condition. Some of the most commonly prescribed medications for postpartum depression include selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac) and sertraline (Zoloft).
It’s important to note that medication alone is not a cure for postpartum depression. It should be used as part of a comprehensive treatment plan that also includes counseling, support groups, and self-care. Creating a warm and loving environment for yourself and your baby can also help in managing the condition.
While medication can be effective in managing postpartum depression, it may take some time for it to start working. It’s crucial to be patient and consistent with your medication, as well as keep your healthcare provider informed about any changes in symptoms or concerns.
If you’re breastfeeding, you should discuss medication options with your healthcare provider. Some medications may be safe to use while breastfeeding, while others may not. Your healthcare provider can help you find the medication that is safe and appropriate for you and your baby.
Remember, everyone’s experience with postpartum depression is unique, and what works for one person may not work for another. It’s important to work closely with your healthcare provider to find the right treatment plan for you.
In addition to medication, other forms of self-care can be helpful in managing postpartum depression. This can include getting regular exercise, eating a balanced diet, getting enough sleep, and finding time to engage in activities you enjoy. Taking breaks and asking for help from friends or family members can also contribute to your overall well-being.
Postpartum depression can feel isolating, but it’s important to remember that you’re not alone. Reach out to your support system, whether it’s a counselor, friend, or support group. International organizations and online communities can also provide a platform for connection and understanding.
Recognize that postpartum depression is a treatable condition, and with the right support and treatment, you can start to feel better. If you’re feeling overwhelmed or hopeless, it’s essential to reach out for help. Your healthcare provider can assist you in making an appointment with a mental health professional who specializes in postpartum depression.
You are not alone in this journey. There are resources available to help you manage postpartum depression and regain your sense of well-being. Don’t hesitate to seek support and take the necessary steps towards recovery.
What are ways to cope with postpartum depression
Postpartum depression is a serious medical condition that affects many new mothers. It is important to recognize the symptoms and seek medical help if you or someone you know is experiencing postpartum depression. Here are some ways to cope with postpartum depression:
1. Seek professional help: Start by talking to your healthcare providers, such as doctors or licensed therapists who specialize in perinatal mental health. They can provide you with information, support, and appropriate treatment options.
2. Join support groups: Connecting with other mothers who have experienced or are currently experiencing postpartum depression can be helpful. Support groups provide a safe space to share your feelings, learn coping strategies, and gain emotional support from others who understand what you’re going through.
3. Stay connected: Reach out to friends and family members who can offer support and understanding. Regularly communicate with loved ones, whether through phone calls, video chats, or in-person visits (when appropriate), to maintain social connections and feel less isolated.
4. Practice self-care: Taking care of yourself is essential for your well-being. Make sure to prioritize activities that bring you joy and help you relax. This could include practicing mindfulness or meditation, engaging in hobbies, exercising, getting enough sleep, and eating well-balanced meals.
5. Educate yourself: Learn more about postpartum depression to better understand its causes, symptoms, and treatment options. Being knowledgeable about the condition can empower you to recognize and address any potential symptoms and seek help when needed.
6. Consider medication: In some cases, doctors may prescribe medication to help manage the symptoms of postpartum depression. Discuss the potential benefits and risks with a healthcare professional to determine if medication is an appropriate option for you.
7. Create a support network: Surround yourself with a network of supportive individuals who can offer practical help, such as assisting with household chores or caring for the baby. Having a strong support system can also provide emotional reassurance and help alleviate feelings of overwhelm.
8. Practice self-compassion: Be kind to yourself and recognize that postpartum depression is not your fault. It is a medical condition that can affect anyone, regardless of their circumstances. Give yourself permission to ask for help and prioritize your well-being.
9. Stay positive: Try to focus on the positive aspects of motherhood and celebrate small victories. Engage in activities that you enjoy with your baby, such as reading to them, playing, and cuddling. Building a warm and loving connection with your baby can have a positive impact on your mental health.
10. Reach out for professional help: If your symptoms worsen or you have thoughts of self-harm or harming your baby, seek immediate medical attention. Postpartum depression can sometimes lead to postpartum psychosis, which requires immediate medical intervention.
Remember, postpartum depression is a treatable condition, and with the right support and treatment, you can navigate through this challenging period and regain your well-being.
What happens if postpartum depression isn’t treated
If postpartum depression, also known as PPD, isn’t treated, it can have serious consequences for the mother, baby, and entire family. Here are some of the potential effects:
- Impaired bonding: Postpartum depression can affect a mother’s ability to bond with her baby. This can lead to difficulties in forming a strong emotional connection and may affect the baby’s emotional well-being.
- Increased risk of long-term depression: Untreated PPD can increase the risk of developing long-term depression. Studies have shown that women who experience PPD are more likely to have a recurrence of depression in the future.
- Negative impact on the baby’s development: PPD can affect a baby’s cognitive and emotional development. Research suggests that infants of mothers with untreated PPD may have delays in language development, problems with social interaction, and lower IQ scores.
- Strain on relationships: Postpartum depression can put a strain on a mother’s relationship with her partner and other family members. It can cause feelings of resentment, anger, and frustration, making it difficult to maintain healthy relationships.
- Increased risk of harming oneself or others: In severe cases, untreated PPD can increase the risk of self-harm or harm towards others. It’s important to seek immediate attention if you or someone you know is experiencing thoughts of hurting themselves or others.
It’s also worth noting that postpartum depression can affect a mother’s physical health. Untreated PPD has been linked to higher levels of stress hormones, which can have short and long-term effects on the body. This includes an increased risk of heart disease, weakened immune system, and potential changes in brain chemistry.
Recognizing the symptoms and seeking treatment for postpartum depression is crucial. If you or anyone you know is experiencing symptoms of PPD, reaching out to a healthcare provider or a community support group can be a helpful first step. Treatment options may include therapy, medication, and lifestyle changes.
Talking about your feelings and fears openly with loved ones can also be a lifeline during this challenging time. Remember, seeking help is not a sign of weakness – it’s a brave step towards regaining your well-being and ensuring the best possible outlook for you, your baby, and your family.
Prevention
Preventing postpartum depression is crucial for the well-being of both the mother and the baby. Although it is not possible to completely eliminate the risk of developing postpartum depression, there are steps that can be taken to reduce the likelihood and severity of the condition.
One of the most important steps in prevention is building a strong support system. A woman should have people she can trust, such as her partner, family, or friends, who can provide emotional support during this time of transition. Beyond the immediate support network, it is also important to connect with other women who have experienced postpartum depression. Joining local or online support groups can be helpful in finding understanding and advice from others who have gone through or are going through similar experiences.
It is also essential to take care of the physical and emotional well-being of the mother. Eating a balanced diet and ensuring that the body receives the necessary nutrients can positively impact the mood. Getting enough sleep, even if it means adjusting to the newborn’s sleep patterns, is crucial. Regular exercise, when the body is ready, can also have a positive effect on both the physical and mental state.
Education and preparation during pregnancy can go a long way in preventing postpartum depression. Attending childbirth and parenting classes can help parents-to-be feel more confident and prepared for the arrival of their baby. Learning about the changes that occur in a woman’s body and mind after childbirth can help manage expectations and reduce feelings of being overwhelmed.
Healthcare providers play a critical role in preventing and identifying postpartum depression. Regular check-ups during pregnancy and after birth are essential for monitoring the physical and emotional well-being of the mother. Providers should screen for postpartum depression using validated screening forms, and offer immediate help and support to anyone who may be experiencing symptoms or is at high risk.
Overall, prevention of postpartum depression involves a combination of emotional support, self-care, education, and professional support. By addressing these factors, the risks and severity of postpartum depression can be reduced, allowing women to enjoy the joys of motherhood without the burden of this serious condition.
Can postpartum depression be prevented
Postpartum depression is a common condition that affects many new mothers. It can cause feelings of extreme sadness, fatigue, and loneliness, and can have a significant impact on a woman’s outlook and relationships. While postpartum depression cannot always be prevented, there are steps you can take to reduce your risk and increase your chances of maintaining good mental health during this challenging time.
1. Build a support network: Connect with other new mothers in your community or join a support group. It can be helpful to talk to other women who are going through similar experiences and understand what you’re going through. Additionally, having friends and family members who can provide emotional support can make a big difference in your well-being.
2. Take care of yourself: It’s important to prioritize self-care after giving birth. Remember to eat well, exercise, and get enough rest. If possible, try to find time for activities you enjoy or hobbies that help you relax and recharge.
3. Communicate with your healthcare provider: Make sure to discuss any concerns or symptoms you’re experiencing with your doctor or midwife. They can help you recognize the signs of postpartum depression and provide guidance and treatment options if necessary. Your pediatrician can also be a valuable resource if you have concerns about your child’s well-being.
4. Be realistic: Understand that the arrival of a new baby can be a stressful and challenging time. It’s normal to feel tired, overwhelmed, and frustrated at times. Be gentle with yourself and don’t expect everything to be perfect. Setting realistic expectations can help alleviate some of the pressure you may be feeling.
5. Seek professional help: If you’re experiencing severe or prolonged symptoms of postpartum depression, don’t hesitate to reach out for additional support. There are specialized treatment centers and clinicians who can provide therapy or prescribe medication if necessary. These professionals can help you develop coping mechanisms, manage stress, and regain balance in your life.
6. Practice skin-to-skin contact: Skin-to-skin contact with your baby has been shown to release hormones that can improve your mood and overall well-being. It has also been linked to better sleep patterns and bonding between mother and child.
While postpartum depression can be a challenging condition to navigate, it’s important to know that you’re not alone and there are resources available to help. By taking proactive steps, including building a support network, practicing self-care, and seeking professional help as needed, you can increase your chances of preventing or effectively managing postpartum depression. Remember, your mental health is just as important as your physical health, and taking care of yourself is essential for the well-being of both you and your child.
Outlook Prognosis
Postpartum depression can have varying levels of severity and can affect different groups of women. Some women may experience mild symptoms that last for a short period of time, while others may develop more extreme symptoms that persist for longer periods.
It is important to seek help and support as soon as possible if you or someone you know is experiencing postpartum depression. Screening tests can quickly determine if you are experiencing postpartum depression or a similar mood disorder.
With proper diagnosis and treatment, many women can recover from postpartum depression and go on to live healthy, fulfilling lives. Medications and counseling can be effective in treating postpartum depression.
Building a strong support system is also crucial. Surrounding yourself with people who understand and can offer help can make a big difference in your recovery. Reach out to loved ones, friends, or support groups to talk about your experiences and seek guidance.
Taking care of your body and mind is essential. Get plenty of rest, eat nutritious meals, and engage in activities that you enjoy. Exercise has been shown to improve mood and relieve symptoms of depression.
Bonding with your baby and developing a secure attachment is another important task during this time. Hold your baby, talk to them, and make eye contact. Touch and physical contact release oxytocin, a hormone that promotes feelings of love and trust.
It is important to be honest with yourself and others about how you are feeling. Don’t be afraid to ask for help or reach out to healthcare professionals. Remember, postpartum depression is not your fault, and there is no shame in seeking treatment.
Feeding and caring for your baby can also be challenging when experiencing postpartum depression. If you are having difficulty with breastfeeding or other aspects of parenting, ask for assistance from a lactation consultant or parenting support center.
Try to keep a routine and establish a sense of normalcy. This can help you feel more in control and reduce feelings of fear and loneliness. Establishing a consistent sleep schedule can also improve your mental well-being.
Lastly, be kind to yourself. It’s normal to have ups and downs as a new parent, especially when dealing with postpartum depression. Remember that you are doing the best you can, and it’s okay to ask for help.
What is the outlook for women with postpartum depression
Postpartum depression is a serious mental health condition that affects many women after the birth of their child. The outlook for women with postpartum depression can vary, but it is important to know that there is hope and help available.
Many women with postpartum depression feel scared and overwhelmed, especially if they are not familiar with the condition. Partners and loved ones can play a crucial role in providing support and understanding during this time.
It is normal for new mothers to experience changes in sleep patterns and shorter periods of sleep after the arrival of a new baby. However, when these changes become severe and interfere with daily functioning, it is important to seek medical help. Doctors and healthcare providers are trained in recognizing the signs and symptoms of postpartum depression and can provide the necessary support and treatment.
One of the first steps in seeking help is through screening and assessment. Many healthcare providers offer these screenings as part of routine postpartum care. They may include questions about physical and emotional well-being. It is important to answer these questions honestly and openly, as they can help determine the best course of action.
Treatment for postpartum depression can vary and may include individual therapy sessions, support groups, or medication. Some women may find that making lifestyle changes, such as incorporating exercise and healthy eating, can help alleviate symptoms. Others may find that relaxation techniques, such as meditation or deep breathing exercises, can be beneficial in managing anxiety and depressive symptoms.
It is important to note that postpartum depression is a treatable condition. With the right support and treatment, many women experience a decrease in symptoms and an improvement in their overall well-being.
In addition to seeking medical care, there are a few self-help strategies that women with postpartum depression can try. These include getting enough rest, eating a balanced diet with plenty of nutrients, and engaging in activities that bring joy and happiness.
Having a strong support system in place, including family, friends, and healthcare providers, can make a significant difference in a woman’s recovery journey. It is important to reach out and ask for help when needed.
In conclusion, while postpartum depression can be a challenging experience, there is hope for recovery. By seeking help, adjusting to life with a new baby, and making self-care a priority, women with postpartum depression can overcome this condition and lead fulfilling lives.
Living With
Living with postpartum depression can be challenging, but there are ways to cope and improve your mental well-being. Regardless of the type of depression someone experiences, it is important to seek help and support from healthcare professionals.
One option to consider is counseling or therapy. Talking to a mental health professional can provide a safe space to discuss your feelings and concerns. They can offer guidance and support as you navigate through this difficult time.
It’s also helpful to educate yourself about postpartum depression. Learning about the different types of depression and understanding the possible effects it can have on a woman’s mental health can be empowering. This knowledge can also help you manage expectations and take steps to improve your overall well-being.
Support groups can be a lifeline for many women experiencing postpartum depression. Connecting with others who have similar experiences can help you feel less alone. These groups offer a sense of community, where you can share your worries, ask questions, and receive support from others who understand what you’re going through.
Some women find that self-care activities help improve their mental well-being. Taking care of your physical health, such as eating a healthy diet and getting regular exercise, can have a positive impact on your mood. It’s also important to make time for activities you enjoy and to practice relaxation techniques to manage stress.
If you have a partner or a supportive network, leaning on them for help and understanding can make a significant difference. Let them know how you’re feeling and what you need. Having a strong support system can provide a sense of comfort and stability.
As hormones and sleep disruptions can contribute to postpartum depression, it’s important to take care of your physical well-being. Making sure you get enough rest, maintaining a balanced diet, and staying hydrated can have a positive impact on your mental health.
Remember that postpartum depression is not your fault. It’s a real medical condition that requires treatment and support. Seeking help is a sign of strength, and there are resources available to help you on your journey towards recovery.
If you or someone you know is struggling with postpartum depression, it’s essential to reach out to a healthcare professional or a helpline. There are online and phone sources available that can offer guidance and support. Never hesitate to ask for help if you need it.
When should I seek professional medical treatment for symptoms related to postpartum depression?

Postpartum depression is a common condition that affects many new mothers. It is important to seek professional medical treatment if you are experiencing symptoms that last beyond the normal “baby blues” period, typically around two weeks after childbirth.
If you find it harder to enjoy activities you used to like or have difficulty bonding with your baby, it may be a sign of postpartum depression. Other symptoms can include feeling moody or irritable, crying frequently without any apparent reason, and having trouble sleeping or sleeping too much.
It’s normal to feel tired and overwhelmed in the early weeks after giving birth, but if these feelings persist or become more extreme, it’s important to reach out for help. Contact your physician or a mental health professional if you are worried about your own mental health or the safety of yourself or your baby.
Recognize that postpartum depression is not your fault. It is a real medical condition that affects many women after childbirth. It can be caused by hormonal changes, such as a sudden decrease in estrogen and progesterone levels, as well as by the physical and emotional stress of caring for a newborn.
Seeking professional medical treatment is crucial because there are effective forms of treatment available. Your healthcare provider may recommend therapy, medication, or a combination of both. Antidepressants can be helpful in managing symptoms, and therapy can provide you with tools to cope with postpartum depression.
In addition to seeking professional medical treatment, there are also self-care strategies you can practice to help manage your symptoms. Take the time to care for yourself by getting enough sleep, eating well, and engaging in activities that bring you joy and relaxation.
Reach out to your support network for help, whether it’s your partner, family, or friends. Don’t be afraid to ask for assistance with household chores, errands, or caring for your baby. It’s important to have moments of self-care and to not isolate yourself.
Researchers have found that skin-to-skin contact with your baby, breastfeeding, and engaging in activities like meditation or deep breathing can increase the release of oxytocin, a hormone associated with bonding and feelings of well-being. These activities can also help decrease feelings of stress and anxiety.
If you are unsure whether your symptoms are related to postpartum depression or are in need of immediate medical attention, it’s best to err on the side of caution and contact a healthcare professional. They can perform tests to assess your hormone levels and overall well-being, and guide you towards appropriate treatment.
The most important thing is to reach out for help when you need it. Postpartum depression is a common and treatable condition, and seeking professional medical treatment can make a positive difference in your well-being and your ability to enjoy the journey of motherhood.
Additional Common Questions
Within the context of postpartum depression, there are often questions that arise regarding various aspects of its causes, treatments, and effects. Here are some additional common questions that you may have:
|
1. Can postpartum depression be treated without medication? Yes, postpartum depression can be treated without medication. In many cases, counseling and therapy sessions can provide effective support and help women cope with their depression. |
|
2. Can postpartum depression affect both mothers and fathers? Yes, postpartum depression can affect both mothers and fathers. While it is more commonly experienced by mothers, fathers can also experience postpartum depression due to the hormonal changes and emotional challenges that come with having a new child. |
|
3. Is it safe to take antidepressants while breastfeeding? While some antidepressants can be passed through breast milk, many are considered safe to use while breastfeeding. However, it is important to discuss the options with your healthcare provider to find the best medication that does not affect the baby’s health. |
|
4. How can I manage my sleep deprivation while dealing with postpartum depression? Managing sleep deprivation can be difficult, especially when dealing with postpartum depression. It is important to prioritize rest and try to get as much sleep as possible. Seek support from your partner, family, or friends to care for the baby while you take naps or rest. Establishing a sleep schedule can also help. |
|
5. What are some additional tips for coping with postpartum depression? Other than seeking therapy and medication, there are several tips that may help in coping with postpartum depression. These include reaching out to support groups, engaging in activities and hobbies that you enjoy, eating well-balanced meals, maintaining regular contact with loved ones, and practicing self-care. |
Remember, it is important to trust yourself and prioritize your own mental health. If you have any further questions or concerns, contacting your healthcare provider is always recommended.
Do I have postpartum anxiety or postpartum depression
Postpartum anxiety and postpartum depression are two common mood disorders that can occur after childbirth. While they share some similarities, they are distinct conditions that require different forms of treatment. In this article, we will discuss the differences between postpartum anxiety and postpartum depression and provide tips on how to manage these conditions.
Postpartum anxiety: Postpartum anxiety is characterized by excessive worrying, racing thoughts, and feeling on edge. It is more than just the usual stress and worry that comes with bringing a new baby into the world. Women with postpartum anxiety may experience frequent panic attacks and have an intense fear that harm will come to their baby. They may also have trouble sleeping, as their mind is constantly racing.
Postpartum depression: Postpartum depression, on the other hand, is a more severe form of mood disorder. It is characterized by feelings of sadness, emptiness, and a loss of interest in activities. Women with postpartum depression may also experience changes in appetite, sleep disturbances, and have difficulty bonding with their baby. They may have recurring thoughts of harming themselves or their baby and may lack energy to perform everyday tasks.
If you are not sure whether you are experiencing postpartum anxiety or postpartum depression, it is important to reach out for help. It is common for women to experience a mix of both conditions, and a professional can provide a proper diagnosis and recommend appropriate treatment options.
When it comes to managing postpartum anxiety and postpartum depression, there are several tips that may help:
| 1 | Take breaks: It’s important to take breaks and practice self-care. Ask a friend or family member to watch the baby so you can have some time for yourself. |
| 2 | Get enough sleep: Sleep deprivation can make the symptoms of postpartum anxiety and depression worse. Try to get as much rest as possible, even if it means taking short naps throughout the day. |
| 3 | Seek professional help: If your symptoms are severe or persistent, do not hesitate to seek professional help. There are many behavioral therapies and medications that can help manage these conditions. |
| 4 | Reach out for support: Talk to someone you trust about what you are going through. Whether it’s a friend, family member, or support group, having someone to lean on can make a big difference. |
| 5 | Consider medication: In some cases, medication may be necessary to manage postpartum anxiety or depression. Talk to your healthcare provider about the option of taking medication to help balance your hormone levels and improve your mental health. |
Remember, you are not alone in your experience. Postpartum anxiety and postpartum depression are common, and many women have faced similar challenges. Regardless of the form of treatment you choose, it’s important to prioritize your mental health and seek the support you need.
Can dads get postpartum depression?

Postpartum depression is commonly associated with mothers, but it can also affect fathers. While it may not receive as much attention, paternal postpartum depression is a real and serious condition that should not be ignored.
According to doctors, around 10% of new fathers experience some form of postpartum depression. However, due to societal expectations and cultural norms, it often goes unrecognized and unaddressed. Many fathers may not even realize they are experiencing depression or may be reluctant to seek help.
Like mothers, fathers can experience mood swings, extreme fatigue, changes in appetite, and difficulty concentrating. They may also face feelings of sadness, irritability, and loss of interest in activities they once enjoyed. These depressive symptoms can begin any time during the first year of parenthood and can last for several months.
It’s important for both partners to understand that postpartum depression is not a sign of weakness or failure. It is a medical condition that can be caused by a combination of hormonal changes, lack of sleep, and the stress of adjusting to life with a new baby.
If a father is experiencing postpartum depression, it’s crucial for him to seek help. This can be in the form of therapy, counseling, or even just talking to a healthcare provider. It’s essential to reach out as soon as possible, as untreated depression can affect not only the father’s well-being but also the overall family dynamic.
While it may be challenging to recognize the signs of postpartum depression in fathers, it’s important for partners and loved ones to be supportive and understanding. Offering a listening ear, encouraging self-care, and providing assistance with daily tasks can make a significant difference in helping a father cope with postpartum depression.
There are also preventive measures fathers can take to manage their mental health during the postpartum period. These include maintaining a healthy sleep schedule, engaging in physical activity to release endorphins, and seeking professional advice or joining support groups specifically for fathers experiencing postpartum depression.
It’s crucial for society to recognize that postpartum depression can affect anyone involved in the caregiving process, not just the mother. By increasing awareness and understanding, we can provide the necessary support and resources for both mothers and fathers who may be affected by this condition.
If you or someone you know is experiencing postpartum depression, do not hesitate to reach out to a healthcare professional or a mental health hotline. You are not alone, and help is available.
What is postpartum dysphoria
Postpartum dysphoria, also known as postpartum depression, is a psychological condition that affects some women after having children. It is different from the “baby blues,” which are common and generally go away after a short time. Postpartum dysphoria is more severe and can last for several weeks or even months.
Postpartum dysphoria happens due to hormonal changes in a woman’s body after giving birth. It can also be influenced by other factors such as lack of sleep, a lack of support, or a history of depression. It is important to recognize the signs of postpartum dysphoria and seek help from a healthcare provider or a mental health professional if needed.
Some common signs of postpartum dysphoria include feeling guilty, having difficulty bonding with the baby, feeling panicked or overwhelmed, having a decreased or loss of interest in activities once enjoyed, changes in appetite and sleeping patterns, and experiencing frequent mood swings.
There are several ways to cope with postpartum dysphoria. Counseling or therapy can be helpful in providing support and guidance. Antidepressant medications may also be recommended in certain cases. It is important to remember that postpartum dysphoria is not the woman’s fault and seeking help is a sign of strength.
In addition to seeking professional help, there are also some self-care practices that can help women cope with postpartum dysphoria. These include taking time for oneself, practicing relaxation techniques such as meditation or deep breathing, getting support from loved ones or joining support groups, and engaging in activities that bring joy and happiness.
Skin-to-skin contact with the baby and bonding activities can also increase feelings of well-being. Taking care of one’s physical health by eating well, exercising, and getting enough restful sleep can also contribute to overall mental well-being.
If you or someone you know is experiencing postpartum dysphoria, it is important to seek help as soon as possible. Many healthcare providers, nurses, and postpartum support centers have resources and expertise in helping women cope with postpartum depression. Remember, you are not alone and there is support available.
| Signs of postpartum dysphoria include: | Ways to cope with postpartum dysphoria include: |
|---|---|
| – Feeling guilty | – Counseling or therapy |
| – Difficulty bonding with the baby | – Antidepressant medications |
| – Feeling panicked or overwhelmed | – Taking time for oneself |
| – Decreased or loss of interest in activities | – Practicing relaxation techniques |
| – Changes in appetite and sleeping patterns | – Getting support from loved ones or support groups |
| – Frequent mood swings | – Engaging in activities that bring joy |
How can I help someone with postpartum depression
Postpartum depression is a serious medical condition that affects many women after childbirth. It can cause a wide range of emotions, from feelings of sadness and worthlessness to anxiety and guilt. If you know someone who is experiencing postpartum depression, there are several things you can do to support them and help them through this difficult time.
1. Be there to listen – One of the most important things you can do is simply be there to listen. Let them know that you are there for them, and encourage them to talk about their feelings. Sometimes, just talking about what they are going through can be a big relief.
2. Offer your help – Postpartum depression can make even the simplest tasks feel overwhelming. Offer to help with household chores, cooking, or taking care of the baby. By offering your assistance, you can help alleviate some of the stress and pressure they may be feeling.
3. Encourage self-care – It’s important for someone with postpartum depression to take care of their physical and mental health. Encourage them to get enough rest, eat healthy, and exercise if possible. Suggest activities they used to enjoy before the baby, such as going for a walk, meditating, or doing something they find relaxing.
4. Be understanding – It’s crucial to be understanding and patient with someone who is experiencing postpartum depression. They may not have the same level of energy or enthusiasm as usual, and their emotions may be all over the place. Try to be supportive and avoid making them feel guilty about their feelings.
5. Educate yourself – Take the time to educate yourself about postpartum depression. Learn about the symptoms, the different types of treatments available, and how it can affect not only the mother but also other family members. The more you know, the better equipped you will be to offer support.
6. Encourage professional help – If the symptoms of postpartum depression persist or worsen, encourage the person to seek professional help. A healthcare provider, such as an OBGYN, can offer guidance and recommend appropriate treatments, such as therapy or medication.
7. Stay connected – Keep in touch with the person regularly, even if it’s just through phone calls or text messages. Postpartum depression can lead to feelings of isolation and distancing from loved ones. Let them know that you’re there for them and that they’re not alone.
8. Offer hope – Postpartum depression can make it difficult for someone to see the light at the end of the tunnel. Remind them that with time, support, and proper treatment, they will start to feel better. Offer stories of others who have successfully managed their postpartum depression and come out on the other side.
9. Be aware of warning signs – It’s important to be aware of the warning signs that someone with postpartum depression may display. These can include sudden changes in mood, loss of interest in daily activities, difficulty bonding with the baby, or thoughts of self-harm. If you notice any of these signs, it’s essential to seek immediate medical attention.
Remember, postpartum depression is a serious medical condition, and even though it may not always be easy to know what to do or say, your support can make a big difference. Your presence and understanding can help someone with postpartum depression feel supported and less alone during this challenging time.
How to Manage and Cope with Postpartum Depression
Postpartum depression can be a challenging experience, but there are ways to manage and cope with it. If you’re finding it difficult to handle your emotions and are frequently feeling low or panicked, it’s important to seek help and not suffer in silence.
One effective strategy is to find a community of other new mothers who are going through similar experiences. Being able to talk openly about your feelings with those who understand can provide a sense of support and relief. Online forums, support groups, and local parenting centers can be great resources for connecting with others.
Though it may be hard, reaching out for help and access to professional support is crucial. Many people believe that seeking help is a sign of weakness, but in reality, it shows strength and the ability to prioritize your well-being and the well-being of your child. A healthcare provider, such as a therapist or psychiatrist, can offer guidance and expertise for managing postpartum depression.
In some cases, medication may be prescribed to help manage postpartum depression. Medications that regulate serotonin reuptake, like selective serotonin reuptake inhibitors (SSRIs), can be effective in balancing mood and reducing symptoms. However, it’s important to note that medication isn’t the best option for everyone and should only be used under the guidance of a healthcare provider.
In addition to seeking professional help, implementing self-care strategies can also be beneficial. Engaging in activities that bring you joy and practicing self-compassion can help combat feelings of low self-esteem and self-worth. This can include things like exercise, socializing with loved ones, getting enough sleep, eating well, and doing activities you enjoy, like hobbies or creative outlets.
Another common symptom of postpartum depression is difficulty sleeping and increased fatigue. Prioritizing sleep and practicing good sleep hygiene can help improve your overall well-being. Creating a nighttime routine, reducing screen time before bed, and using relaxation techniques like deep breathing or mindfulness exercises can all contribute to better sleep quality.
It’s important to understand that you’re not alone in facing postpartum depression. Many other new mothers go through the same challenges and can relate to what you’re experiencing. Remember that seeking help is not a sign of weakness, but a brave and proactive step towards better mental health.
If you or someone you know is struggling with postpartum depression, don’t hesitate to seek help. Reach out to a healthcare provider, talk to friends and family, or connect with support groups in your community. Remember that you don’t have to face this alone.